Ready to get certified?
Free CDCES Coach App

Subscribe
eNewsletter
Download
Free Med Pocket Cards
Rationale of the Week | Lifestyle Therapy for MASLD and MASH
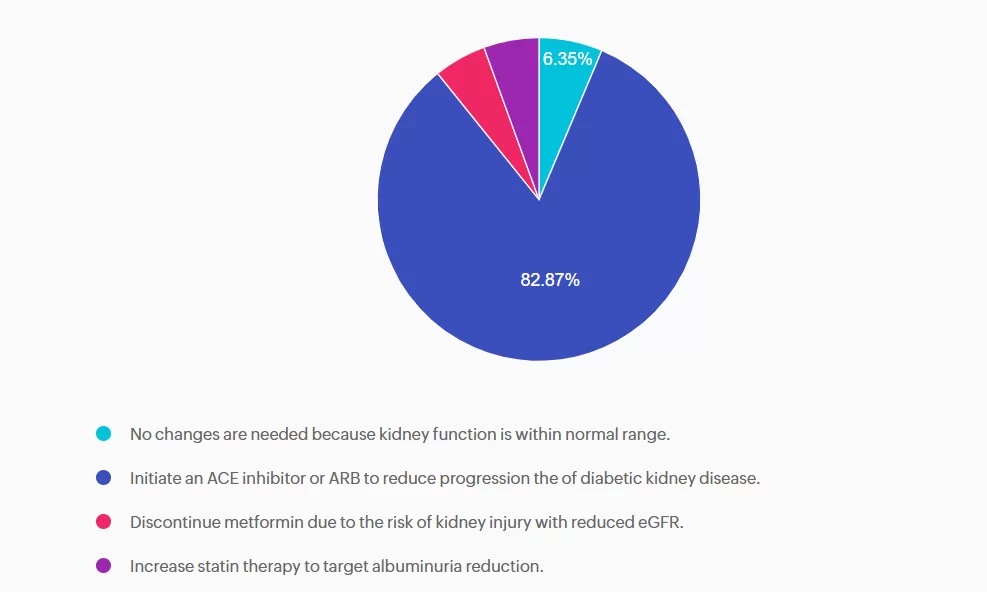
For last week’s practice question, we quizzed participants on Lifestyle Therapy for MASLD and MASH. 83% of respondents chose the best answer. We want to clarify and share this important information, so you can pass it on to people living with diabetes and your colleagues, plus prepare for exam success!
Before we start though, if you don’t want any spoilers and haven’t tried the question yet, you can answer it below: Answer Question

PJ has had type 2 diabetes for 8 years and is here for a follow-up visit. Labs indicate A1c at 7.2%, lipids at target, eGFR of 78 mL/min/1.73m², and urine albumin-to-creatinine ratio (UACR) of 65 mg/dL. Blood pressure at the office visit today was 142/86, which is consistent with home monitored values. PJ confirms taking medications, metformin and simvastatin. PJ inquires about recently completed lab work.
According to the ADA Standards of Care, what would be an appropriate next step in the diabetes care plan?
- No changes are needed because kidney function is within normal range.
- Initiate an ACE inhibitor or ARB to reduce progression the of diabetic kidney disease.
- Discontinue metformin due to the risk of kidney injury with reduced eGFR.
- Increase statin therapy to target albuminuria reduction.
Getting to the Best Answer
Answer A is incorrect: 6.35% chose this answer, “No changes are needed because kidney function is within normal range.” A is incorrect. Although eGFR indicates stage 2 kidney disease, the elevated UACR, ≥30 mg/g, confirms moderately increased risk and recommendation to treat. Additionally, PJ’s blood pressure is also above the target. Intervention is needed to protect kidney and cardiovascular health.
Answer B is correct: 83% chose this answer, “Initiate an ACE inhibitor or ARB to reduce progression the of diabetic kidney disease.” PJ has a mildly decreased eGFR, but UACR is elevated above 30 mg/g, indicating a recommendation to treat. Additionally, intervention is needed to optimize blood pressure. According to the ADA Standards of Care in Diabetes, individuals with diabetes, hypertension, and moderately increased albuminuria should be treated with an ACE inhibitor or angiotensin receptor blocker. The use of sodium-glucose cotransporter 2 (SGLT2) inhibitors or glucagon-like peptide 1 agonists (GLP1-RA), with demonstrated benefits, could also be considered to reduce CKD progression.
Answer C is incorrect: 5.25% chose this answer, “Discontinue metformin due to the risk of kidney injury with reduced eGFR.” Metformin is safe to continue unless eGFR falls below 30 30 mL/min/1.73m². PJ’s kidney function is adequate for continued use. However, consideration to add a change to SGLT2 or GLP1 with kidney benefit could also promote additional A1c reduction.
Answer D is incorrect: 5.52% chose this answer, “Increase statin therapy to target albuminuria reduction.” Statins are recommended for ASCVD prevention, but they do not reduce albuminuria. Lipids are within normal range, and albuminuria should be addressed with an ACE inhibitor/ARB or potentially a SGLT2 inhibitor or GLP-1 RA.
We hope you appreciate this week’s rationale! Thank you so much for taking the time to answer our Question of the Week and participate in this fun learning activity!

Invite a colleague to our DiabetesEd Seminar in San Diego and get $75 off each registration.
Use code FriendDiscountSD during check out to save.
Join us live in San Diego October 22nd – 23rd, 2025 for our upcoming
DiabetesEd Training Seminar
30+ CEs with Expanded Accreditation!

Join our expert team for engaging, interactive sessions that bring the ADA Standards of Care to life—covering medications, behavior change, technology, and more. Ideal for CDCES or BC-ADM exam prep, this course also includes a 4-hour Virtual Medical Nutrition Therapy Toolkit and bonus content that also meets CDCES renewal requirements.
Program Objectives:
Upon completion of this activity, participants should be able to:
- Describe the current ADA Standards for diagnosis, goals, and person-centered diabetes management across the lifespan.
- Demonstrate insulin pattern management and dosing strategies in clinical scenarios.
- Implement timely screening and risk reduction strategies for microvascular and cardiovascular complications.
- Incorporate behavior change techniques and medical nutrition therapy to support people with diabetes self-management and lifestyle adjustment.
Expert Faculty:

Diana Isaacs, PharmD, BCPS, BCACP, CDCES, BC-ADM, FADCES, FCCPCES

Beverly Thomassian, RN, MPH, CDCES, BC-ADM
Faculty Bios & Disclosures
Our expert team transforms complex diabetes science into clear, practical insights—keeping it real, engaging, and fun!
Program Faculty Disclosures:
Partners for Advancing Clinical Education (Partners) requires every individual in a position to control educational content to disclose all financial relationships with ineligible companies that have occurred within the past 24 months. Ineligible companies are organizations whose primary business is producing, marketing, selling, re-selling, or distributing healthcare products used by or on patients.
All relevant financial relationships for anyone with the ability to control the content of this educational activity are listed below and have been mitigated according to Partners policies. Others involved in the planning of this activity have no relevant financial relationships.
Faculy Bios & Disclosures:
 Coach Beverly Thomassian RN, MPH, CDCES, BC-ADM – CEO of DiabetesEd Services
Coach Beverly Thomassian RN, MPH, CDCES, BC-ADM – CEO of DiabetesEd ServicesDisclosures:
Beverly Thomassian has no financial disclosures
Bio:
 Diana Isaacs, PharmD, BCPS, BCACP, CDCES, BC-ADM, FADCES, FCCPCES
Diana Isaacs, PharmD, BCPS, BCACP, CDCES, BC-ADM, FADCES, FCCPCES
Disclosures:
Dr. Diana Isaacs has the following relevant financial relationships:
- Consultant, advisor, and speaker for Abbot Labratories, Dexcom, Medtronic, Insulet, Lilly, Cequr, Sanofi, and Undermyfork
- Board member at Association for Diabetes Care and Education Specialists
Bio:
Diana Isaacs was awarded 2020 ADCES Diabetes Educator of the Year for her educational platform promoting the use of CGM for people with diabetes and other innovations. She serves in leadership roles for several pharmacies and diabetes organizations. She has numerous diabetes publications and research projects with a focus on medications, CGM and diabetes technology.
For the past three year, Dr. Isaacs has served as a contributing author for the 2023 ADA Standards of Care.
As the Program Coordinator and clinical pharmacist specialist in the Cleveland Clinic Diabetes Center, Dr. Isaacs brings a wealth of clinical knowledge combined with extensive research and speaking experience to this program.
Expanded Accreditation
Activity Start and End Date: 10/22/25 – 10/23/2025
Estimated time to complete the activity: 15 hours and 30 minutes
_____________________________________
Jointly provided by Partners for Advancing Clinical Education and Diabetes Education Services
![]()
![]()
Joint Accreditation Statement:
 In support of improving patient care, this activity has been planned and implemented by Partners for Advancing Clinical Education (Partners) and Diabetes Education Services. Partners is jointly accredited by the Accreditation Council for Continuing Medical Education (ACCME), the Accreditation Council for Pharmacy Education (ACPE), and the American Nurses Credentialing Center (ANCC), to provide continuing education for the healthcare team.
In support of improving patient care, this activity has been planned and implemented by Partners for Advancing Clinical Education (Partners) and Diabetes Education Services. Partners is jointly accredited by the Accreditation Council for Continuing Medical Education (ACCME), the Accreditation Council for Pharmacy Education (ACPE), and the American Nurses Credentialing Center (ANCC), to provide continuing education for the healthcare team.
Physician Continuing Education:
Partners designates this enduring material for a maximum of 15.50 AMA PRA Category 1 Credit(s)™. Physicians should claim only the credit commensurate with the extent of their participation in the activity.
Nursing Continuing Professional Development:
The maximum number of hours awarded for this Nursing Continuing Professional Development activity is 15.50 contact hours.
Pharmacy Continuing Education:
Partners designates this continuing education activity for 15.50 contact hour(s) (1.550 CEUs) of the Accreditation Council for Pharmacy Education.
(Universal Activity Number – JA4008073-9999-25-206-L01-P)
Type of Activity: Application
For Pharmacists: Upon successfully completing the activity evaluation form, transcript information will be sent to the NABP CPE Monitor Service within 4 weeks.
Dietitian Continuing Education:
This program offers 15.50 CPEUs for dietitians.
Interprofessional Continuing Education:
![]() This activity was planned by and for the healthcare team, and learners will receive 15.50 Interprofessional Continuing Education (IPCE) credit for learning and change.
This activity was planned by and for the healthcare team, and learners will receive 15.50 Interprofessional Continuing Education (IPCE) credit for learning and change.
For additional information about the accreditation of this activity, please visit https://partnersed.com.
The use of DES products does not guarantee the successful passage of the certification exam. CBDCE and ADCES do not endorse any preparatory or review materials for the CDCES or BC-ADM exams, except for those published by CBDCE & ADCES.
Question of the Week | Which Treatment is FDA Approved for MASH?

MJ just discovered that in addition to their type 2 diabetes and a BMI of 31, they also have MASH.
Based on this diagnosis, which FDA approved medication would help address their steatosis?
- Semaglutide (Ozempic)
- Empagliflozin (Jardiance)
- Tirzepatide (Mounjaro)
- Semaglutide (Wegovy)

Invite a colleague to our DiabetesEd Seminar in San Diego and get $75 off each registration.
Use code FriendDiscountSD during check to save.
Join us live in San Diego October 22nd – 23rd, 2025 for our upcoming
DiabetesEd Training Seminar
Earn 30+ CEs with Expanded Accreditation!
Join our expert team for engaging, interactive sessions that bring the ADA Standards of Care to life—covering medications, behavior change, technology, and more. Ideal for CDCES or BC-ADM exam prep, this course also includes a 4-hour Virtual Medical Nutrition Therapy Toolkit and bonus content that also meets CDCES renewal requirements.

Program Objectives:
Upon completion of this activity, participants should be able to:
- Describe the current ADA Standards for diagnosis, goals, and person-centered diabetes management across the lifespan.
- Demonstrate insulin pattern management and dosing strategies in clinical scenarios.
- Implement timely screening and risk reduction strategies for microvascular and cardiovascular complications.
- Incorporate behavior change techniques and medical nutrition therapy to support people with diabetes self-management and lifestyle adjustment.
Expert Faculty:

Diana Isaacs, PharmD, BCPS, BCACP, CDCES, BC-ADM, FADCES, FCCPCES

Beverly Thomassian, RN, MPH, CDCES, BC-ADM
Faculty Bios & Disclosures
Our expert team transforms complex diabetes science into clear, practical insights—keeping it real, engaging, and fun!
Program Faculty Disclosures:
Partners for Advancing Clinical Education (Partners) requires every individual in a position to control educational content to disclose all financial relationships with ineligible companies that have occurred within the past 24 months. Ineligible companies are organizations whose primary business is producing, marketing, selling, re-selling, or distributing healthcare products used by or on patients.
All relevant financial relationships for anyone with the ability to control the content of this educational activity are listed below and have been mitigated according to Partners policies. Others involved in the planning of this activity have no relevant financial relationships.
Faculy Bios & Disclosures:
 Coach Beverly Thomassian RN, MPH, CDCES, BC-ADM – CEO of DiabetesEd Services
Coach Beverly Thomassian RN, MPH, CDCES, BC-ADM – CEO of DiabetesEd ServicesDisclosures:
Beverly Thomassian has no financial disclosures
Bio:
 Diana Isaacs, PharmD, BCPS, BCACP, CDCES, BC-ADM, FADCES, FCCPCES
Diana Isaacs, PharmD, BCPS, BCACP, CDCES, BC-ADM, FADCES, FCCPCES
Disclosures:
Dr. Diana Isaacs has the following relevant financial relationships:
- Consultant, advisor, and speaker for Abbot Labratories, Dexcom, Medtronic, Insulet, Lilly, Cequr, Sanofi, and Undermyfork
- Board member at Association for Diabetes Care and Education Specialists
Bio:
Diana Isaacs was awarded 2020 ADCES Diabetes Educator of the Year for her educational platform promoting the use of CGM for people with diabetes and other innovations. She serves in leadership roles for several pharmacies and diabetes organizations. She has numerous diabetes publications and research projects with a focus on medications, CGM and diabetes technology.
For the past three year, Dr. Isaacs has served as a contributing author for the 2023 ADA Standards of Care.
As the Program Coordinator and clinical pharmacist specialist in the Cleveland Clinic Diabetes Center, Dr. Isaacs brings a wealth of clinical knowledge combined with extensive research and speaking experience to this program.
Expanded Accreditation
Activity Start and End Date: 10/22/25 – 10/23/2025
Estimated time to complete the activity: 15 hours and 30 minutes
_____________________________________
Jointly provided by Partners for Advancing Clinical Education and Diabetes Education Services
![]()
![]()
Joint Accreditation Statement:
 In support of improving patient care, this activity has been planned and implemented by Partners for Advancing Clinical Education (Partners) and Diabetes Education Services. Partners is jointly accredited by the Accreditation Council for Continuing Medical Education (ACCME), the Accreditation Council for Pharmacy Education (ACPE), and the American Nurses Credentialing Center (ANCC), to provide continuing education for the healthcare team.
In support of improving patient care, this activity has been planned and implemented by Partners for Advancing Clinical Education (Partners) and Diabetes Education Services. Partners is jointly accredited by the Accreditation Council for Continuing Medical Education (ACCME), the Accreditation Council for Pharmacy Education (ACPE), and the American Nurses Credentialing Center (ANCC), to provide continuing education for the healthcare team.
Physician Continuing Education:
Partners designates this enduring material for a maximum of 15.50 AMA PRA Category 1 Credit(s)™. Physicians should claim only the credit commensurate with the extent of their participation in the activity.
Nursing Continuing Professional Development:
The maximum number of hours awarded for this Nursing Continuing Professional Development activity is 15.50 contact hours.
Pharmacy Continuing Education:
Partners designates this continuing education activity for 15.50 contact hour(s) (1.550 CEUs) of the Accreditation Council for Pharmacy Education.
(Universal Activity Number – JA4008073-9999-25-206-L01-P)
Type of Activity: Application
For Pharmacists: Upon successfully completing the activity evaluation form, transcript information will be sent to the NABP CPE Monitor Service within 4 weeks.
Dietitian Continuing Education:
This program offers 15.50 CPEUs for dietitians.
Interprofessional Continuing Education:
![]() This activity was planned by and for the healthcare team, and learners will receive 15.50 Interprofessional Continuing Education (IPCE) credit for learning and change.
This activity was planned by and for the healthcare team, and learners will receive 15.50 Interprofessional Continuing Education (IPCE) credit for learning and change.
For additional information about the accreditation of this activity, please visit https://partnersed.com.
The use of DES products does not guarantee the successful passage of the certification exam. CBDCE and ADCES do not endorse any preparatory or review materials for the CDCES or BC-ADM exams, except for those published by CBDCE & ADCES.
October 2025 eNews
Featured Articles ___________________________ |
Upcoming Programs ___________________________
Upcoming FREE Webinars ___________________________ |
Happy October!💚
Greetings, wonderful healthcare colleagues!
With the onset of fall, it is the perfect time to curl up with a good book and read our monthly newsletter. Pull out your calendar and save the dates for our upcoming courses and free webinars.
First up, you are going to do a happy dance when you download our GLP-1/GIP Indications Cheat Sheet. With a glance, you will be able to quickly determine which incretin is the best match for the person sitting across from you, considering their glucose levels, weight goals, age, and other co-conditions. Shout out to Diana Issacs, PharmD, CDCES, for getting the ball rolling on this latest addition to our Cheat Sheet Library.
Speaking of Diana Isaacs, you won’t want to miss her at our DiabetesEd Course in San Diego in a few weeks. We have so much fun co-teaching at this conference and giving attendees our full attention! Invite a friend, save $75, and get ready for a wonderful experience and a comprehensive diabetes update.
Over 60% of people with diabetes are living with liver steatosis. Our nutrition expert, Christine Craig, reviews evidence-based lifestyle approaches that you can quickly apply in your clinical practice.
If you are looking for an easy-to-use insulin delivery device, check out this review article on CeQur Simplicity by our tech expert, Dr. Sarah Beattie. She explores the benefits and limitations of this straightforward bolus insulin delivery device.
A big welcome to our newest team member and customer service advocate, Astraea Ballinger. They bring a wealth of experience and positive energy to the team, and we are thrilled to introduce them.
Test your knowledge with our question and rationale of the week, and we hope to see you in San Diego!
With appreciation,
Coach Beverly, Bryanna, Astraea & Katarina

Save $75 – Invite a colleague to our DiabetesEd Seminar in San Diego.
Use code FriendDiscountSD during checkout to save!
Join us live in San Diego October 22nd - 23rd, 2025 for our upcoming
DiabetesEd Training Seminar
30+ CEs with Expanded Accreditation!

Join our expert team for engaging, interactive sessions that bring the ADA Standards of Care to life—covering medications, behavior change, technology, and more. Ideal for CDCES or BC-ADM exam prep, this course also includes a 4-hour Virtual Medical Nutrition Therapy Toolkit and bonus content that also meets CDCES renewal requirements.
Program Objectives:
Upon completion of this activity, participants should be able to:
- Describe the current ADA Standards for diagnosis, goals, and person-centered diabetes management across the lifespan.
- Demonstrate insulin pattern management and dosing strategies in clinical scenarios.
- Implement timely screening and risk reduction strategies for microvascular and cardiovascular complications.
- Incorporate behavior change techniques and medical nutrition therapy to support people with diabetes self-management and lifestyle adjustment.
Expert Faculty:

Diana Isaacs, PharmD, BCPS, BCACP, CDCES, BC-ADM, FADCES, FCCPCES

Beverly Thomassian, RN, MPH, CDCES, BC-ADM
Faculty Bios & Disclosures
Our expert team transforms complex diabetes science into clear, practical insights—keeping it real, engaging, and fun!
Program Faculty Disclosures:
Partners for Advancing Clinical Education (Partners) requires every individual in a position to control educational content to disclose all financial relationships with ineligible companies that have occurred within the past 24 months. Ineligible companies are organizations whose primary business is producing, marketing, selling, re-selling, or distributing healthcare products used by or on patients.
All relevant financial relationships for anyone with the ability to control the content of this educational activity are listed below and have been mitigated according to Partners policies. Others involved in the planning of this activity have no relevant financial relationships.
Faculy Bios & Disclosures:
 Coach Beverly Thomassian RN, MPH, CDCES, BC-ADM – CEO of DiabetesEd Services
Coach Beverly Thomassian RN, MPH, CDCES, BC-ADM – CEO of DiabetesEd ServicesDisclosures:
Beverly Thomassian has no financial disclosures
Bio:
 Diana Isaacs, PharmD, BCPS, BCACP, CDCES, BC-ADM, FADCES, FCCPCES
Diana Isaacs, PharmD, BCPS, BCACP, CDCES, BC-ADM, FADCES, FCCPCES
Disclosures:
Dr. Diana Isaacs has the following relevant financial relationships:
- Consultant, advisor, and speaker for Abbot Labratories, Dexcom, Medtronic, Insulet, Lilly, Cequr, Sanofi, and Undermyfork
- Board member at Association for Diabetes Care and Education Specialists
Bio:
Diana Isaacs was awarded 2020 ADCES Diabetes Educator of the Year for her educational platform promoting the use of CGM for people with diabetes and other innovations. She serves in leadership roles for several pharmacies and diabetes organizations. She has numerous diabetes publications and research projects with a focus on medications, CGM and diabetes technology.
For the past three year, Dr. Isaacs has served as a contributing author for the 2023 ADA Standards of Care.
As the Program Coordinator and clinical pharmacist specialist in the Cleveland Clinic Diabetes Center, Dr. Isaacs brings a wealth of clinical knowledge combined with extensive research and speaking experience to this program.
Expanded Accreditation
Activity Start and End Date: 10/22/25 – 10/23/2025
Estimated time to complete the activity: 15 hours and 30 minutes
_____________________________________
Jointly provided by Partners for Advancing Clinical Education and Diabetes Education Services
![]()
![]()
Joint Accreditation Statement:
 In support of improving patient care, this activity has been planned and implemented by Partners for Advancing Clinical Education (Partners) and Diabetes Education Services. Partners is jointly accredited by the Accreditation Council for Continuing Medical Education (ACCME), the Accreditation Council for Pharmacy Education (ACPE), and the American Nurses Credentialing Center (ANCC), to provide continuing education for the healthcare team.
In support of improving patient care, this activity has been planned and implemented by Partners for Advancing Clinical Education (Partners) and Diabetes Education Services. Partners is jointly accredited by the Accreditation Council for Continuing Medical Education (ACCME), the Accreditation Council for Pharmacy Education (ACPE), and the American Nurses Credentialing Center (ANCC), to provide continuing education for the healthcare team.
Physician Continuing Education:
Partners designates this enduring material for a maximum of 15.50 AMA PRA Category 1 Credit(s)™. Physicians should claim only the credit commensurate with the extent of their participation in the activity.
Nursing Continuing Professional Development:
The maximum number of hours awarded for this Nursing Continuing Professional Development activity is 15.50 contact hours.
Pharmacy Continuing Education:
Partners designates this continuing education activity for 15.50 contact hour(s) (1.550 CEUs) of the Accreditation Council for Pharmacy Education.
(Universal Activity Number – JA4008073-9999-25-206-L01-P)
Type of Activity: Application
For Pharmacists: Upon successfully completing the activity evaluation form, transcript information will be sent to the NABP CPE Monitor Service within 4 weeks.
Dietitian Continuing Education:
This program offers 15.50 CPEUs for dietitians.
Interprofessional Continuing Education:
![]() This activity was planned by and for the healthcare team, and learners will receive 15.50 Interprofessional Continuing Education (IPCE) credit for learning and change.
This activity was planned by and for the healthcare team, and learners will receive 15.50 Interprofessional Continuing Education (IPCE) credit for learning and change.
For additional information about the accreditation of this activity, please visit https://partnersed.com.
The use of DES products does not guarantee the successful passage of the certification exam. CBDCE and ADCES do not endorse any preparatory or review materials for the CDCES or BC-ADM exams, except for those published by CBDCE & ADCES.
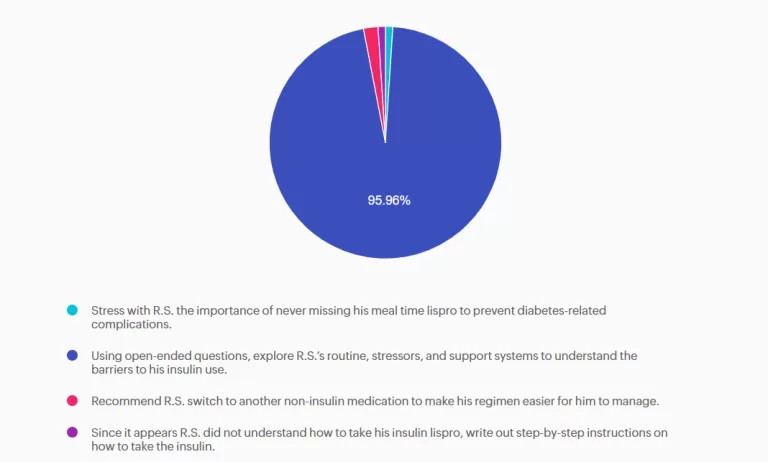
Rationale of the Week | Grandfather Avoiding Bolus Insulin
For last week’s practice question, we quizzed participants on insulin. 96% of respondents chose the best answer. We want to clarify and share this important information, so you can pass it on to people living with diabetes and your colleagues, plus prepare for exam success!
Before we start though, if you don’t want any spoilers and haven’t tried the question yet, you can answer it below: Answer Question

R.S. is a 60-year-old with type 2 diabetes who was recently placed on insulin lispro at meals. He has taken insulin glargine once a day for five years. Previously, non-insulin medications have been ineffective or not tolerated. He continues to have hyperglycemia despite the addition of insulin lispro. During his diabetes education visit today, he shared that he has not been taking his mealtime insulin lispro because he does not want to inject it in front of his grandchildren, who live with him. He feels overwhelmed by these additional injections but wants to get his blood glucose levels under better control so he can have the energy to play with his grandchildren and avoid losing his eyesight like his mother did.
As the diabetes care and education specialist, which of the following would be the most appropriate first step in addressing R.S.’s concerns?
- Stress with R.S. the importance of never missing his meal time lispro to prevent diabetes-related complications.
- Using open-ended questions, explore R.S.’s routine, stressors, and support systems to understand the barriers to his insulin use.
- Recommend R.S. switch to another non-insulin medication to make his regimen easier for him to manage.
- Since it appears R.S. did not understand how to take his insulin lispro, write out step-by-step instructions on how to take the insulin.
Getting to the Best Answer
Answer A is incorrect: 1% chose this answer, “Stress with R.S. the importance of never missing his meal time lispro to prevent diabetes-related complications.” R.S. is aware that his glycemic control is important, and he is already aware of the risk of diabetes-related complications. Counseling him on this would not help him be successful with his insulin management.
Answer B is correct: 96% chose this answer, “Using open-ended questions, explore R.S.’s routine, stressors, and support systems to understand the barriers to his insulin use.” R.S. is struggling with barriers to successful insulin management. A holistic approach would be to ask open-ended questions about his current routine, stressors, and support systems to gain a better understanding of these barriers. This information can lead to a personalized plan of care to help improve glycemic control.
Answer C is incorrect: 2% chose this answer, “Recommend R.S. switch to another non-insulin medication to make his regimen easier for him to manage.” He has already attempted other non-insulin therapies, and these were either ineffective or not tolerated. Changing his regimen would not be successful at improving his glycemic control and quality of life.
Answer D is incorrect: 1% chose this answer, “Since it appears R.S. did not understand how to take his insulin lispro, write out step-by-step instructions on how to take the insulin.” R.S. appears to understand how to take his insulin lispro at meals. Writing out the instructions would not improve his situation. It is not a lack of knowledge, but the multiple barriers in his life that are keeping him from being able to implement this new medication regimen.
We hope you appreciate this week’s rationale! Thank you so much for taking the time to answer our Question of the Week and participate in this fun learning activity!

Invite a colleague to our DiabetesEd Seminar in San Diego and get $75 off each registration.
Use code FriendDiscountSD during check out to save.
Join us live in San Diego October 22nd – 23rd, 2025 for our upcoming
DiabetesEd Training Seminar
30+ CEs with Expanded Accreditation!

Join our expert team for engaging, interactive sessions that bring the ADA Standards of Care to life—covering medications, behavior change, technology, and more. Ideal for CDCES or BC-ADM exam prep, this course also includes a 4-hour Virtual Medical Nutrition Therapy Toolkit and bonus content that also meets CDCES renewal requirements.
Program Objectives:
Upon completion of this activity, participants should be able to:
- Describe the current ADA Standards for diagnosis, goals, and person-centered diabetes management across the lifespan.
- Demonstrate insulin pattern management and dosing strategies in clinical scenarios.
- Implement timely screening and risk reduction strategies for microvascular and cardiovascular complications.
- Incorporate behavior change techniques and medical nutrition therapy to support people with diabetes self-management and lifestyle adjustment.
Expert Faculty:

Diana Isaacs, PharmD, BCPS, BCACP, CDCES, BC-ADM, FADCES, FCCPCES

Beverly Thomassian, RN, MPH, CDCES, BC-ADM
Faculty Bios & Disclosures
Our expert team transforms complex diabetes science into clear, practical insights—keeping it real, engaging, and fun!
Program Faculty Disclosures:
Partners for Advancing Clinical Education (Partners) requires every individual in a position to control educational content to disclose all financial relationships with ineligible companies that have occurred within the past 24 months. Ineligible companies are organizations whose primary business is producing, marketing, selling, re-selling, or distributing healthcare products used by or on patients.
All relevant financial relationships for anyone with the ability to control the content of this educational activity are listed below and have been mitigated according to Partners policies. Others involved in the planning of this activity have no relevant financial relationships.
Faculy Bios & Disclosures:
 Coach Beverly Thomassian RN, MPH, CDCES, BC-ADM – CEO of DiabetesEd Services
Coach Beverly Thomassian RN, MPH, CDCES, BC-ADM – CEO of DiabetesEd ServicesDisclosures:
Beverly Thomassian has no financial disclosures
Bio:
 Diana Isaacs, PharmD, BCPS, BCACP, CDCES, BC-ADM, FADCES, FCCPCES
Diana Isaacs, PharmD, BCPS, BCACP, CDCES, BC-ADM, FADCES, FCCPCES
Disclosures:
Dr. Diana Isaacs has the following relevant financial relationships:
- Consultant, advisor, and speaker for Abbot Labratories, Dexcom, Medtronic, Insulet, Lilly, Cequr, Sanofi, and Undermyfork
- Board member at Association for Diabetes Care and Education Specialists
Bio:
Diana Isaacs was awarded 2020 ADCES Diabetes Educator of the Year for her educational platform promoting the use of CGM for people with diabetes and other innovations. She serves in leadership roles for several pharmacies and diabetes organizations. She has numerous diabetes publications and research projects with a focus on medications, CGM and diabetes technology.
For the past three year, Dr. Isaacs has served as a contributing author for the 2023 ADA Standards of Care.
As the Program Coordinator and clinical pharmacist specialist in the Cleveland Clinic Diabetes Center, Dr. Isaacs brings a wealth of clinical knowledge combined with extensive research and speaking experience to this program.
Expanded Accreditation
Activity Start and End Date: 10/22/25 – 10/23/2025
Estimated time to complete the activity: 15 hours and 30 minutes
_____________________________________
Jointly provided by Partners for Advancing Clinical Education and Diabetes Education Services
![]()
![]()
Joint Accreditation Statement:
 In support of improving patient care, this activity has been planned and implemented by Partners for Advancing Clinical Education (Partners) and Diabetes Education Services. Partners is jointly accredited by the Accreditation Council for Continuing Medical Education (ACCME), the Accreditation Council for Pharmacy Education (ACPE), and the American Nurses Credentialing Center (ANCC), to provide continuing education for the healthcare team.
In support of improving patient care, this activity has been planned and implemented by Partners for Advancing Clinical Education (Partners) and Diabetes Education Services. Partners is jointly accredited by the Accreditation Council for Continuing Medical Education (ACCME), the Accreditation Council for Pharmacy Education (ACPE), and the American Nurses Credentialing Center (ANCC), to provide continuing education for the healthcare team.
Physician Continuing Education:
Partners designates this enduring material for a maximum of 15.50 AMA PRA Category 1 Credit(s)™. Physicians should claim only the credit commensurate with the extent of their participation in the activity.
Nursing Continuing Professional Development:
The maximum number of hours awarded for this Nursing Continuing Professional Development activity is 15.50 contact hours.
Pharmacy Continuing Education:
Partners designates this continuing education activity for 15.50 contact hour(s) (1.550 CEUs) of the Accreditation Council for Pharmacy Education.
(Universal Activity Number – JA4008073-9999-25-206-L01-P)
Type of Activity: Application
For Pharmacists: Upon successfully completing the activity evaluation form, transcript information will be sent to the NABP CPE Monitor Service within 4 weeks.
Dietitian Continuing Education:
This program offers 15.50 CPEUs for dietitians.
Interprofessional Continuing Education:
![]() This activity was planned by and for the healthcare team, and learners will receive 15.50 Interprofessional Continuing Education (IPCE) credit for learning and change.
This activity was planned by and for the healthcare team, and learners will receive 15.50 Interprofessional Continuing Education (IPCE) credit for learning and change.
For additional information about the accreditation of this activity, please visit https://partnersed.com.
The use of DES products does not guarantee the successful passage of the certification exam. CBDCE and ADCES do not endorse any preparatory or review materials for the CDCES or BC-ADM exams, except for those published by CBDCE & ADCES.
High Five for Fiber

Dietary fiber is a complex carbohydrate and bioactive food compound that has an important role in diabetes management and cardiometabolic health. High-fiber dietary patterns are associated with a lower risk of type 2 diabetes, cardiovascular disease, obesity, gastrointestinal disorders, and certain cancers. ¹,²
In individuals with diabetes, fiber-rich eating patterns have been shown to improve glycemia, reduce postprandial glucose excursions, and improve lipid profiles. ¹ A recent meta-analysis found that for individuals with type 1 diabetes, a high- fiber diet not only supports A1c reduction but is also associated with reduced hypoglycemia risk due to its role in slowing digestion and absorption. ³ Despite this evidence most adults fail to meet recommended fiber intake guidelines, presenting an opportunity for nutrition interventions.
Dietary Fiber and Diabetes
The Dietary Reference Intake (DRI) for fiber, established by the Institute of Medicine, along with the 2026 ADA Standards of Care ¹ , recommends 14 grams of fiber per 1,000 Calories, corresponding to an Adequate Intake of approximately 25–38 grams per day depending on age, gender, and energy needs. 4 Higher-fiber dietary patterns greater than 35 grams per day ³ and up to 50 grams per day 1 may provide additional glycemic benefits for individuals with diabetes.
Both the 2020–2025 and 2025–2030 Dietary Guidelines for Americans 5 emphasize fruits, vegetables, whole grains, and legumes as primary fiber sources; however, the recommended portions of these food groups differ between guidelines. The newly released 2025–2030 guidelines place greater emphasis on overall dietary patterns and whole-food sources, with reduced total grain servings, increased emphasis on legumes, and a prioritization of reduced processed foods rather than focusing on fiber as an isolated nutrient.
However, the Scientific Report of the guidelines does reference an optimal fiber intake range of 25–29 grams per day. ² Aligning with ADA Standards of Care, the focus shifts from individual nutrients to overall eating patterns, supporting health professionals to encourage food choices that help individuals meet evidence-based guidelines for fiber recommendations.
Disparities Occurring With Dietary Fiber Intake
Despite serving-size guidance and scientific evidence on the benefits of fiber, average intake in the United States remains far below recommendations. Fewer than 5-7% of adults meet daily fiber requirements. 5 Disparities in intakes among groups have grown over time, with data from the 2017–2018 USDA Economic Research Service showing that, within Hispanic populations, fiber consumption was highest at about 9 grams per 1,000 Calories, compared with
7.7 grams per 1,000 Calories among non-Hispanic White individuals, and 7.0 grams per 1,000 Calories among Black individuals 6 .
Although the amount varies across groups, most individuals reach only 58% of the daily fiber recommendations. Inadequate intake stems from not only food preferences but tolerance, food cost and access, time constraints, nutrition literacy, as well as, other social determinants of health. To help the U.S. population meet fiber goals, practical strategies consider not only culturally relevant nutrition interventions but food assistance programs, systems planning, and community resources that improve access to fiber-rich foods.
Understanding Fiber: “Good Source” Versus “Excellent Source”
Therapeutically, the type of fiber matters, with insoluble or soluble providing different health benefits. Insoluble fiber creates bulk within the stool and can promote bowel regularity and reduces risk of certain cancers. Whereas, soluble fiber forms a viscous gel in the gastrointestinal tract and provides metabolic benefits, including reduced postprandial glucose responses and lower cholesterol levels. 7
While not specific to type, understanding fiber claims on food labels is a practical entry point for guiding individuals toward higher-fiber food choices. According to FDA labeling regulations, foods may be labeled a “good source” of fiber if they provide 10–19% of the Daily Value per serving (≥3 grams), while an “excellent source” of fiber provides greater than or equal to 20% of the Daily Value per serving (≥5 grams). 8
Additionally, the FDA has approved the use of “will reduce the risk of coronary heart disease” health claims
on food packaging due the cardioprotective effects of high soluble fibers β-glucan (found in oats and barley) and psyllium. 9 Emphasizing dietary patterns, food quality assessment, label literacy, and considerations for additional functional fiber supplementation can support individuals with diabetes to make informed food choices and shifts in their intake.
Practical Strategies & Ideas to Implement Higher Fiber Intake
Practical strategies to promote higher fiber intake are outlined in the 2026 ADA Standards of Care¹ (Check out Nutrition Behaviors to Encourage ¹ within section 5: Facilitating Positive Health Behaviors and Well-being to Improve Health Outcomes) and can be reinforced through simple, actionable “High-Five for Fiber” tips.
These tips are a catchy way to encourage health behaviors that may help individuals gradually add fiber (slow addition improves gut tolerance) to meet daily recommendations. Ideas can include having individuals choose at least one “high- fiber, excellent source” daily (which has more than 5 g fiber per serving), discover high soluble fiber foods, strive for five, or more, servings from vegetables and/or fruits each day, and/or “take five” to plan meals that include whole grains, fruits, vegetables, legumes, and/or nuts and seeds each week. These tips encourage choice, helping individuals find foods that fit their personal preferences, affordability, cultural traditions, and lifestyles ¹ while supporting sustainable, health-promoting dietary patterns.
High-Five Food Ideas:
- Chickpeas (6 grams per ½ cup cooked)
- Black beans (6 grams per ½ cup cooked)
- Lentils (8 grams per ½ cup cooked)
- Black-eyed peas (5 grams per ½ cup cooked)
- Raspberries (8 grams per 1 cup)
- Blackberries (8 grams per 1 cup)
- Avocado (6 grams per ½ medium)
- Brussels sprouts (5 grams per 1 cup cooked)
- Artichoke (6 grams per ½ medium cooked)
- Boiled collard greens (5 grams per 1 cup cooked)
- Chia seeds (6 grams per 2 tablespoons)
- Barley (6 grams per 1 cup cooked)
- Whole wheat pita (~ 5 grams fiber per 1 pita)
References:
- American Diabetes Association Professional Practice Committee for Diabetes. 5. Facilitating Positive Health Behaviors and Well-being to Improve Health Outcomes: Standards of Care in Diabetes—2026. Diabetes Care 1 January 2026; 49
(Supplement_1): S89–S131. https://doi.org/10.2337/dc26-S005 - Guo Y, Li M, Huang Y. Association of dietary fiber intake with all-cause and cardiovascular mortality in U.S. adults with metabolic syndrome: NHANES 1999–2018. Front Nutr. 2025;12:1659000. doi:10.3389/fnut.2025.1659000.
- Zeng J, Beck M, Barouti AA, Löfvenborg JE, Carlsson S, Lampousi AM. Effects of different dietary patterns on glucose management in type 1 diabetes: a systematic review and meta-analysis of randomized controlled trials. EClinicalMedicine. 2025 Apr 28;83:103222. doi:10.1016/j.eclinm.2025.103222.
- Institute of Medicine (US) Committee to Review Dietary Reference Intakes. Summary Tables. Washington, DC: National Academies Press (US); 2011. Accessed January 18, 2026. https://www.ncbi.nlm.nih.gov/books/NBK56068/table/summarytables.t4/?report=objectonly
- U.S. Department of Health and Human Services (HHS) & U.S. Department of Agriculture (USDA) (2026). Dietary Guidelines for Americans, 2025–2030.
- Guthrie J, Lin BH, Smith TA. Food Consumption and Nutrient Intake Trends Emerge Over Past Four Decades. U.S. Department of Agriculture, Economic Research Service. August 28, 2024. Accessed January 18, 2026. https://www.ers.usda.gov/amber-waves/2024/august/food-consumption-and-nutrient-intake-trends-emerge-over-past-four-decades/
- McRorie JW Jr, McKeown NM. Understanding the Physics of Functional Fibers in the Gastrointestinal Tract: An Evidence-Based Approach to Resolving Enduring Misconceptions about Insoluble and Soluble Fiber. J Acad Nutr Diet. 2017
Feb;117(2):251-264. doi: 10.1016/j.jand.2016.09.021. - Food and Drug Administration, Department of Health and Human Services. 21 CFR § 101.54: Nutrient Content Claims for “Good Source,” “High,” “More,” and “High Potency.” Electronic Code of Federal Regulations. Updated through December 31, 2025. Accessed January 18, 2026. https://www.ecfr.gov/current/title-21/chapter-I/subchapter-B/part-101/subpart-D/section-101.54
- U.S. Food and Drug Administration. Authorized Health Claims That Meet the Significant Scientific Agreement (SSA) Standard. FDA. Accessed January 18, 2026.
https://www.fda.gov/food/nutrition-food-labeling-and-critical-foods/authorized-health-claims-meet-significant-scientific-agreement-ssa-standard
Learn More With Upcoming Webinars & Spreading the Love Sale!
Prepare for the CDCES Exam: Get Ready for Success!
Course credits through AMA PRA Category 1 Credits™, ACPE, ANCC, and CDR!
Get exam-ready with confidence.
Our CDCES Boot Camp Online Prep Bundle is a comprehensive, high-impact program built specifically for healthcare professionals preparing for the Certified Diabetes Care and Education Specialist (CDCES) exam who want to level-up their clinical knowledge and skills.
✔ Learn at your pace with expert-led, exam-focused content
✔ Everything you need—organized, practical, and in one place
✔ Perfect for self-directed learners who want complete, person-centered content for clinical practice and exam prep.
✔ Build knowledge, sharpen test-taking skills, and prepare with confidence—on your schedule.
Focused. Flexible. Proven.
Basic & e-Deluxe CDCES Boot Camp Bundle Includes:
- Levels 1, 2, and 3 of our Online University
- 30+ expert-led courses
- 50 CE/CPEUs
- 400+ online practice questions
- Handouts, podcast, video and one year access—all in one streamlined platform.
Spreading the Love Sale
Save 15% on ALL of Our Online Courses
Use the Code "LOVE15" for 15% Off at Checkout!
Sale Ends on February 16th, 2026!
Rationale of the Week | Keeping You in the Loop: twiist Insulin Pump
For last week’s practice question, we quizzed participants on RT forgetting their insulin, and what would be the best response. % of respondents chose the best answer. We want to clarify and share this important information, so you can pass it on to people living with diabetes and your colleagues, plus prepare for exam success!
Before we start though, if you don’t want any spoilers and haven’t tried the question yet, you can answer it below: Answer Question

Grace is a 38-year-old female who has lived with type 1 diabetes for 20 years. She is a nurse and works variable shifts. She voices concern today about her hemoglobin A1c being elevated at 8.4% over the past 6 months. She is doing everything she can to manage her diet, daily exercise routine, and reports rarely missing insulin doses. She is currently using a Dexcom G7 CGM.
She has never pursued insulin pump therapy because she was fearful that she would no longer be in control of her diabetes if she used a pump. She is now interested in an automated insulin delivery system and asks you which pump is “best” for controlling blood sugar.
What is the best way to answer this question?
- Discuss the insulin pump options that connect with the Dexcom G7 CGM. This will help simplify her transition to pump therapy by minimizing the learning curve when starting an AID system.
- Acknowledge Grace’s interest in insulin pump technology and recommend that she wait until more advanced insulin pump algorithms are available that are easier to use.
- Recommend that Grace use a tubeless pump as it will suit her better due to her work as a nurse and active lifestyle. This will help to avoid tubing issues or the insertion site becoming dislodged.
- Review with Grace the details of all the available insulin pumps, algorithms, and compatible CGMs so she can make a personalized decision based on her preferences and lifestyle.
Getting to the Best Answer
Answer A is incorrect: % chose this answer, “Discuss the insulin pump options that connect with the Dexcom G7 CGM. This will help simplify her transition to pump therapy by minimizing the learning curve when starting an AID system.” Although some insulin pumps are compatible with the Dexcom CGM, switching to a different CGM supplier should not restrict clients from selecting the insulin pump that best suits their needs.
Answer B is incorrect: % chose this answer, “Acknowledge Grace’s interest in insulin pump technology and recommend that she wait until more advanced insulin pump algorithms are available that are easier to use.” Automated insulin delivery systems offer advanced automation. Waiting for future technology will not help Grace improve glycemic control now.
Answer C is incorrect: % chose this answer, “Recommend that Grace use a tubeless pump as it will suit her better due to her work as a nurse and active lifestyle. This will help to avoid tubing issues or the insertion site becoming dislodged.” The type of pump, with or without tubing, is a personal decision and is not based solely on occupation.
Answer D is correct: % chose this answer, “Review with Grace the details of all the available insulin pumps, algorithms, and compatible CGMs so she can make a personalized decision based on her preferences and lifestyle.” Choosing the right insulin pump is a highly personalized decision. Each insulin pump has different variables and CGM connectivity that must be considered. Grace will need to be educated on the available options so she can determine which insulin pump will work best for her.
We hope you appreciate this week’s rationale! Thank you so much for taking the time to answer our Question of the Week and participate in this fun learning activity!
Rationale of the Week | MS keeps getting UTI’s – Best action?
For last week’s practice question, we quizzed participants on MS continuously getting UTIs, and what would be the best response. % of respondents chose the best answer. We want to clarify and share this important information, so you can pass it on to people living with diabetes and your colleagues, plus prepare for exam success!
Before we start though, if you don’t want any spoilers and haven’t tried the question yet, you can answer it below: Answer Question

MS is a 59-year-old with type 2 diabetes who is struggling with frequent urinary tract infections. They are on metformin and empagliflozin, and their A1C is 7.3%. MS has already received several courses of antibiotics.
Which of the following actions would you recommend?
- Drink sugar-free cranberry juice a few times a week.
- Apply topical vaginal estrogen cream.
- Get A1C below 7% by adding basal insulin.
- Evaluate MS for autoimmune conditions.
Getting to the Best Answer
Answer A is incorrect: % chose this answer, “Drink sugar-free cranberry juice a few times a week.” Scientific studies have yielded mixed and inconsistent results regarding the effectiveness of cranberry juice for prevention. MS needs an intervention that will provide ongoing relief.
Answer B is correct: % chose this answer, “Apply topical vaginal estrogen cream.” Vaginal estrogen cream can help prevent recurrent urinary tract infections (UTIs) in postmenopausal women by restoring the health of vaginal and urinary tissues. Estrogen helps restore a healthy vaginal pH, increases beneficial bacteria, and improves circulation, creating an environment that is less hospitable to uropathogens. It is a non-antibiotic option recommended by medical societies and is associated with a significant reduction in rUTIs.
Answer C is incorrect: % chose this answer, “Get A1C below 7% by adding basal insulin.” Getting A1C to target can reduce risk of infections, but MS A1C is already close to target. They need an effective treatment for their frequent UTI’s.
Answer D is incorrect: % chose this answer, “Evaluate MS for autoimmune conditions.” Frequent UTIs are not usually associated with autoimmune conditions. MS needs an effective treatment for their frequent UTI’s.
We hope you appreciate this week’s rationale! Thank you so much for taking the time to answer our Question of the Week and participate in this fun learning activity!
Learn more about HRT and UTIs in our blog “Hormone Replacement Therapy (HRT) – What You Need to Know”
Learn More From Our Expert
Dr. Jill Schramm, DNP, FNP-C, BC-ADM, CDCES
Level 5 | Hot Flashes & Hyperglycemia
Recorded and Ready For Viewing!

Meet Medtronic’s New CGM Lineup

Medtronic ended 2025 with a bang, launching three new continuous glucose monitors (CGMs): Instinct, Simplera
Sync TM , and Simplera TM . These FDA-approved CGM options join the already established Medtronic Guardian TM 4 CGM.
Let’s explore the latest Medtronic CGM options to help you match the best CGM for your clients’ needs.
Medtronic CGM Lineup
All of Medtronic’s CGM options function without fingerstick calibrations, making glucose monitoring simpler. Each CGM connects to a specific Medtronic diabetes device to improve glycemic control. While CGM functionality is similar across the lineup, key differences can influence which option is the best fit for your clients.
The Guardian TM 4 was introduced in 2023 and is still available. This sensor requires rechargeable components. It also differs from the newer options in size and insertion
technique.
The Latest Medtronic CGM Options
Guardian TM 4
- Disposable sensor with rechargeable transmitter
- Requires the use of 2 hands to insert
- Up to 7-day wear time
- 2-hour warm-up period
- Approved for ages 7 years old and up
- Compatible with the MiniMed TM 780G system
- Size: 2.0 x 2.6 in
The Instinct, Simplera Sync TM, and Simplera TM are all-in-one, disposable models with no rechargeable components and can be inserted using just one hand. ¹ The smaller size of these options can be a significant factor for clients.
Instinct
- Disposable all-in-one sensor made by Abbot in partnership with Medtronic
- One-handed insertion
- 15-day wear time
- 1 hour warm-up period
- Approved for ages 7 years old and up
- Compatible with the MiniMed TM 780G system
- Compatible with InPen TM smart insulin pen in the MiniMed Go™ system (FDA-approved January 2026, with expected launch later in 2026) ²
- Size: 0.11 x 0.83 in
Simplera Sync TM
- Disposable all-in-one sensor
- One-handed insertion
- 6-day wear time with a 24-hour grace period
- 2-hour warm-up period
- Approved for ages 7 years old and up
- Compatible with the MiniMed TM 780G system
- Size: 0.19 x 1.13 in
Simplera TM
- Disposable all-in-one sensor
- One-handed insertion
- 6-day wear time with a 24-hour grace period
- 2-hour warm-up period
- Approved for ages 18 years old and up
- Compatible with the InPen TM smart insulin pen system
- Size: 0.19 x 1.13 in
Finding the Perfect Match
As diabetes healthcare providers, you are often asked to help navigate CGM choices. To best achieve this, you work with clients to explore their personal preferences, clinical needs, physical limitations, and comfort with technology to find the most appropriate option.
Who may benefit from the new CGM options?
Individuals who are:
- Looking for simpler technology
- Experiencing decreased hand dexterity
- Wanting a smaller, lower-profile sensor
- Preferring a longer wear time
- Seeking a disposable CGM option
As Medtronic CGMs continue to evolve, diabetes healthcare professionals support clients in choosing the option that best suits their needs. Your clinical insight, familiarity with each CGM, and assessment of the individual client’s goals and preferences help ensure that diabetes technology is used as an empowering tool rather than a barrier to care.
References:
- Medtronic. (n.d.). Medtronic continuous glucose monitors (CGM) comparison. https://www.medtronicdiabetes.com/customer-support/sensors-and-transmitters-support/compare-sensors
- Medtronic Diabetes. (2026, January 12). Medtronic Diabetes announces FDA clearance for MiniMed Go™ Smart MDI system featuring Instinct sensor made by Abbott. [Press Release]. https://news.medtronic.com/2026-01-12-Medtronic-Diabetes-announces-FDA-clearance-for-MiniMed-Go-TM-Smart-MDI-system-featuring-Instinct-sensor-made-by-Abbott
Learn More About Type 1 Staging & Stds
With Our CDCES Boot Camp Bundle | Includes Level(s) 1-3!
Welcome to our selection of comprehensive CDCES Boot Camp Online Prep Bundles that are specifically designed for healthcare professionals who are studying for the Certified Diabetes Care and Education Specialist (CDCES) exam.
Course credits through AMA PRA Category 1 Credits™, ACPE, ANCC, and CDR!
We offer a selection of prep bundles to meet everyone’s needs! See the descriptions below to review what is included in each option.
CDCES Boot Camp | Basic Exam Prep Bundle: This option is perfect for someone who wants just the Online Courses and materials all in one place, our Online University. This bundle includes Levels 1, 2, and 3 & Toolkits which equates to over 30 courses, 50 CEs/CPEUs, and 400+ online practice questions.
CDCES Boot Camp | e-Deluxe Exam Prep Bundle: This bundle has all of the courses from the Basic Bundle, along with the ADCES Certification Review Guide Practice Questions e-book with 400+ practice questions.