
Subscribe
eNewsletter

Ready to get certified?
Free CDCES Coach App
Download
Free Med Pocket Cards

AR says they just found out they are pregnant. AR has type 2 diabetes and polycystic ovary syndrome and takes metformin 1000mg BID, semaglutide (Ozempic) 1.0mg weekly, and 30 units glargine insulin for diabetes management. Her most recent A1C was 8.2%. What is the most important action to take?
Click Here to Test your Knowledge

Pregnancy with diabetes is confronted with a variety of issues that require special attention, education, and understanding. This course reviews those special needs while focusing on Gestational Diabetes and Pre-Existing Diabetes. Included are the most recent diagnostic criteria, management goals, and prevention of complications during pregnancy. A helpful review for the CDCES Exam and for those who want more information on people who are pregnant and live with Diabetes.
Objectives:
The use of DES products does not guarantee the successful passage of the CDCES exam. CBDCE does not endorse any preparatory or review materials for the CDCES exam, except for those published by CBDCE.
There are so many amazing and dedicated people and organizations working to revitalize our planet. To make it easy to explore these opportunities, Bryanna and I put together this list with the hope that you find inspiration for action. Thank you.


Please enjoy these FREE resources that we have put together for you:
The use of DES products does not guarantee the successful passage of the CDCES exam. CBDCE does not endorse any preparatory or review materials for the CDCES exam, except for those published by CBDCE.
When I was considering college, my dad offered me some simple advice, “Why don’t you become a nurse?” Four years later, I stood proudly with my white cap and nursing pin securely fastened as an RN graduate.
As I reflect on my years in this noble profession, I have witnessed the most unselfish acts of love and pure heroism by my nursing colleagues. I have highlighted some top qualities that represent my gratitude, but this thank you list could encompass an entire page.
This week is a perfect time to let our nursing colleagues, mentors, professors, and friends know how much they are appreciated.
Coach Beverly thanks each nurse who has cared for me, held my hand, and reassured me that I am going to be okay.

These are just a few ideas to get started. As you think of that special moment of gratitude, maybe you will come up with the perfect idea for that one special nurse.
With gratitude,
Coach Beverly
Sign up for Diabetes Blog Bytes – we post one daily Blog Byte from Monday to Friday. And of course, Tuesday is our Question of the Week. It’s Informative and FREE! Sign up below!
The use of DES products does not guarantee the successful passage of the CDCES exam. CBDCE does not endorse any preparatory or review materials for the CDCES exam, except for those published by CBDCE.

For last week’s practice question, we quizzed test takers on how diabetes and earth health are interconnected. 78% of respondents chose the best answer, GREAT JOB. We want to share this important information, so you can pass it on to people living with diabetes and your colleagues. We can all take action to protect the earth and prepare for extreme climate events.
Before we start though, if you don’t want any spoilers and haven’t tried the question yet, you can answer it below: Answer Question
Question: According to a NIH systematic literature review, there is clear evidence that diabetes and climate change are interconnected. Which of the following situations are due to the impact of a changing climate?
Answer Choices:
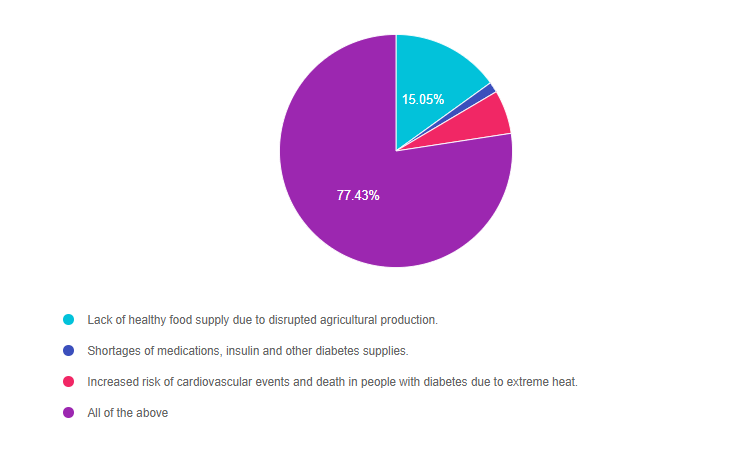
As shown above, the most common choice was option 4, the second most common answer was option 1, then option 3, and finally 2.
Answer one – 15.05% chose this answer, and it is accurate “Lack of healthy food supply due to disrupted agricultural production.” It is true that extreme weather can result in agricultural production disruptions. In our community, many fields that were once green with trees and crops, now are brown and barren. There is not enough water to keep crops alive and growing. When the healthy food supply is limited, people living with diabetes may turn to lower-cost, processed foods which are environmentally unfriendly and low in nutrients.
Answer two – 1.46% of you chose this answer and it is accurate, “Shortages of medications, insulin, and other diabetes supplies.” It is true that with recent climate disasters, like the Camp Fire, Hurricane Katrina in 2005, and Hurricane Harvey in 2017, resulted in people not being able to access, afford or safely store their medications, including insulin. In addition, we are experiencing supply chain disruptions in D50 (25 grams of glucose in a 50 ml prefilled syringe (50% glucose)) to treat hypoglycemia and certain intravenous fluids are in short supply. Other diabetes products and medications could be impacted in the future.
Answer three – 6.07% of respondents chose this answer and it is accurate, “Increased risk of cardiovascular events and death in people with diabetes due to extreme heat.” It is true that people with diabetes are at greater risk of experiencing dehydration and cardiovascular events during periods of extreme heat. With the increasing frequency of extreme heat episodes, there is an associated increased risk of heat-related death and cardiovascular events for people living with diabetes. Several studies reveal that people with diabetes have a higher risk of death on hot days, and are more likely to need emergency care and those with a history of heart disease are most vulnerable.
Finally, Answer four – 77.43% chose this answer, “All of the above.” YES. Great job, all of the answers are true, there is clear evidence that diabetes and climate changes are interconnected. As Diabetes Specialists, I believe we can make a difference by leaning into our unique blend of behavior change skills, advocacy, and scientific knowledge.
We can take a two-fold approach:
This bundle includes our CDCES Online Prep Bundle plus the ADCES Review Guide.
The online bundle includes Level 1, Level 2, and Level 3 (Boot Camp), plus two bonus courses. The ADCES Review Guide offers over 480+ practice questions and is a fantastic independent study tool and comprehensive resource for the Diabetes Care and Education Specialist Exam.
Read More: What is a CDCES? First awarded in 1986, as Certified Diabetes Educator (CDE) credential and in 2020 with a new name: Certified Diabetes Care and Education Specialist (CDCES) to more accurately reflect the specialty. CDCES has become a standard of excellence for the delivery of quality diabetes education. Those who hold this certification are known to possess comprehensive knowledge of and experience in diabetes prevention, management, and prediabetes. “Becoming a Certified Diabetes Care and Education Specialist (CDCES) is one of the best professional and personal decisions I have ever made.” – Coach Beverly Thomassian, RN, MPH, CDCES, BC-ADM 
Read More: 3 Reasons to Become a CDCES “The best part of becoming a CDCES is working with my colleagues and people living with diabetes. As diabetes educators, we hear compelling and beautiful life stories. I am astounded by the barriers they face and inspired by their adaptability, problem-solving skills, and resilience.” Reason 1: CDCES is a widely recognized certification by employers and health care professionals throughout the U.S. This credential demonstrates a specialized and in-depth knowledge in the prevention and treatment of individuals living with pre-diabetes and diabetes. Reason 2: Currently, 10% of people in the U.S. have diabetes and another 35% have pre-diabetes which means 45% of Americans are running around with elevated blood glucose levels. Given this epidemic, there will be plenty of future job opportunities. Reason 3: Having my CDCES along with my nursing degree, has opened many doors of opportunity; from working as an inpatient Diabetes Nurse Specialist in a hospital to working as a Manager of Diabetes Education in the outpatient setting to starting my own consulting company.
Sign up for Diabetes Blog Bytes – we post one daily Blog Byte from Monday to Friday. And of course, Tuesday is our Question of the Week. It’s Informative and FREE! Sign up below!
The use of DES products does not guarantee the successful passage of the CDCES exam. CBDCE does not endorse any preparatory or review materials for the CDCES exam, except for those published by CBDCE.

Like many of you, I have a personal relationship with climate change.
On a blustery day in November 2018, the Camp Fire burned down the hospital and the entire town where I provided diabetes care for over 20 years. In a matter of a short six hours, over 30,000 people who lived in Paradise lost their community and sense of place.
I lost working with my incredible diabetes team and my extended diabetes family. Others lost everything. The Camp Fire has devastated us all in very personal ways. It is considered the deadliest and most destructive wildfire in California history.
Since the town of Paradise was a popular retirement destination, many of those who survived the fiery drive down the hill were frail and elderly. More than 3,000 of them had diabetes and many fled their homes without their meters, insulin, or other critical medications.
With the help of the Red Cross and hundreds of volunteers, we were able to connect most people with needed medications and supplies, but many went without. People with diabetes lost connections to their providers, pharmacies and support systems.
We lost 85 of our beautiful community members due to the fire and thousands of our neighbors dispersed to other states and towns to start their lives over. Over half of our providers moved away and a hospital that provided care to a rural community was suddenly gone. This extreme loss and upheaval reveals the painful truth that we need proactively take action to reduce the frequency and severity of climate disasters and be prepared for future events.
According to a 2020 article published in the Journal of Community Hospital Internal Medicine Perspectives, climate change, and in particular, increasing global temperatures, is expected to impact the health of people living with diabetes and lead to worse outcomes.
After completing a literature review, the authors concluded that diabetes and climate change are interconnected. Let’s explore how.
Hotter Temperatures Worsen Diabetes Outcomes
People with diabetes are at greater risk of experiencing dehydration and cardiovascular events during periods of extreme heat. With the increasing frequency of extreme heat episodes, there is an associated increased risk of heat-related death and cardiovascular events for people living with diabetes. Several studies reveal that people with diabetes have a higher risk of death on hot days, and are more likely to need emergency care and those with a history of heart disease are most vulnerable.
Shortage of Medical Supplies and Medications
Recent climate disasters, like the Camp Fire, Hurricane Katrina in 2005, and Hurricane Harvey in 2017, resulted in people not being able to access, afford or safely store their medications, including insulin. In addition, we are experiencing supply chain disruptions in D50 (25 grams of glucose in a 50 ml prefilled syringe (50% glucose)) to treat hypoglycemia and certain intravenous fluids are in short supply.
Food Supply Shortages
Extreme weather can result in agricultural production disruptions. In our community, many fields that were once green with trees and crops, now are brown and barren. There is not enough water to keep crops alive and growing. This also means job loss and less money flowing into communities. When the healthy food supply is limited, people living with diabetes may turn to lower-cost, processed foods which are environmentally unfriendly and low in nutrients.
Diabetes and climate change are clearly interconnected. Extreme weather events and rising temperatures will significantly impact people living with diabetes, especially those with cardiovascular disease. The disruption in the supply of life-saving medications (e.g. insulin) due to extreme weather combined with decreased access to healthy foods are difficult issues that require problem-solving by individuals, communities, and government leaders.

As Diabetes Specialists, I believe we can make a difference by leaning into our unique blend of behavior change skills, advocacy, and scientific knowledge
We can take a two-fold approach:
A note of hope. Three years after the Camp Fire, people are rebuilding in Paradise. There is a better understanding of the need for preventive forest management and exit routes. However, the longstanding California drought continues to contribute to future fire risk. Water conservation is more important now than ever. We can take action to reverse the heating planet. Read our blog on actions we can start taking today.
Change isn’t easy. We aren’t going for perfect, we are starting with intention and slowly moving to action, giving ourselves lots of grace along the way. I am excited to share my successes and wrong turns with you on this journey and we would love to hear from you too!
Read more on our blog, Earth Day Secrets to Improving Planet Health
Stay tuned and we share details and resources on each of these 10 Steps over the next few months. And, please send us your stories too at [email protected]. We want to hear from you!
Sign up for Diabetes Blog Bytes – we post one daily Blog Byte from Monday to Friday. And of course, Tuesday is our Question of the Week. It’s Informative and FREE! Sign up below!
The use of DES products does not guarantee the successful passage of the CDCES exam. CBDCE does not endorse any preparatory or review materials for the CDCES exam, except for those published by CBDCE.

For older adults with diabetes using insulin therapy, which of the following is the most accurate statement?
Click Here to Test your Knowledge
We are living longer and more people are getting diabetes. The American Diabetes Association has updated the Older Adults Standards, with special attention to considering the reduction of medication and insulin therapy intensity. The older population has unique issues and special needs that require consideration as we provide diabetes self-management education. This online course highlights key areas of assessment, intervention, and advocacy for older clients living with diabetes.
Objectives:
Sign up for Diabetes Blog Bytes – we post one daily Blog Byte from Monday to Friday. And of course, Tuesday is our Question of the Week. It’s Informative and FREE! Sign up below!
The use of DES products does not guarantee the successful passage of the CDCES exam. CBDCE does not endorse any preparatory or review materials for the CDCES exam, except for those published by CBDCE.

We loved celebrating Earth Day with all of you. Your response to our “PocketCard for a Planet Pledge campaign” knocked our socks off. Over 900 people committed to taking action for the Earth. Plus, hundreds of you added our own ideas. We decided to continue the planetary PocketCard party for one more week because we love our community!
This month’s newsletter explores the link between climate change and diabetes from a personal and community level. We provide ideas for prevention, preparation, and actions to take in case of a climate-related disaster. People with diabetes are especially vulnerable during extreme climate events and helping ready them for disasters can save lives.
In addition, we highlight a recent study that demonstrates reducing four risk factors improves outcomes, which is great news to share.
Living with diabetes can be overwhelming. Messages of hope for people with diabetes can provide motivation to continue with self-care during those hard times.
Lastly, I would like to dedicate this newsletter to a very special person. Ruth always showed up to our diabetes support group with the energy of two people and the mental clarity of someone half her age. Around this time of year, she would distribute Emergency Preparedness materials and would carefully review the exit routes out of Paradise in case of fire. She would go around the room and ask each person if they had their emergency bag ready. For each of the seventeen years that I ran that support group before the hospital and town burned down, Ruth gave the same impassioned spiel. I can only imagine how many lives she saved.
May we all embody the spirit of Ruth as we move forward on this journey. With wishes for health and wonderment,
Beverly, Bryanna, Jackson, and Amanda
Featured Articles
Upcoming Webinars
Featured Items
This bundle includes our CDCES Online Prep Bundle plus the ADCES Review Guide.
The online bundle includes Level 1, Level 2, and Level 3 (Boot Camp), plus two bonus courses. The ADCES Review Guide offers over 480+ practice questions and is a fantastic independent study tool and comprehensive resource for the Diabetes Care and Education Specialist Exam.
Read More: What is a CDCES? First awarded in 1986, as Certified Diabetes Educator (CDE) credential and in 2020 with a new name: Certified Diabetes Care and Education Specialist (CDCES) to more accurately reflect the specialty. CDCES has become a standard of excellence for the delivery of quality diabetes education. Those who hold this certification are known to possess comprehensive knowledge of and experience in diabetes prevention, management, and prediabetes. “Becoming a Certified Diabetes Care and Education Specialist (CDCES) is one of the best professional and personal decisions I have ever made.” – Coach Beverly Thomassian, RN, MPH, CDCES, BC-ADM 
Read More: 3 Reasons to Become a CDCES “The best part of becoming a CDCES is working with my colleagues and people living with diabetes. As diabetes educators, we hear compelling and beautiful life stories. I am astounded by the barriers they face and inspired by their adaptability, problem-solving skills, and resilience.” Reason 1: CDCES is a widely recognized certification by employers and health care professionals throughout the U.S. This credential demonstrates a specialized and in-depth knowledge in the prevention and treatment of individuals living with pre-diabetes and diabetes. Reason 2: Currently, 10% of people in the U.S. have diabetes and another 35% have pre-diabetes which means 45% of Americans are running around with elevated blood glucose levels. Given this epidemic, there will be plenty of future job opportunities. Reason 3: Having my CDCES along with my nursing degree, has opened many doors of opportunity; from working as an inpatient Diabetes Nurse Specialist in a hospital to working as a Manager of Diabetes Education in the outpatient setting to starting my own consulting company.
Sign up for Diabetes Blog Bytes – we post one daily Blog Byte from Monday to Friday. And of course, Tuesday is our Question of the Week. It’s Informative and FREE! Sign up below!
The use of DES products does not guarantee the successful passage of the CDCES exam. CBDCE does not endorse any preparatory or review materials for the CDCES exam, except for those published by CBDCE.

For last week’s practice question, we quizzed test takers on which labs to order for JR. 57% of respondents chose the best answer. We want to share this important information, so you can pass it on to people living with diabetes and your colleagues, plus prepare for exam success!
Before we start though, if you don’t want any spoilers and haven’t tried the question yet, you can answer it below: Answer Question
Question: JR’s mom has type 1 diabetes and JR’s dad has type 2 diabetes. JR is 21 years old and in the emergency room with a glucose of 482 mg/dl. Besides checking glucose, ketones and A1C levels, which of the following lab test can be used to determine if someone has autoimmune diabetes?
Answer Choices:
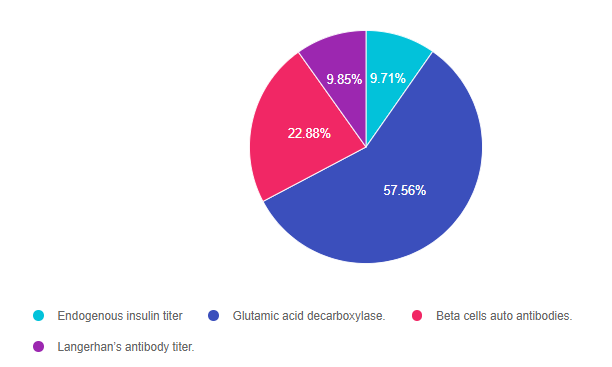
As shown above, the most common choice was option 2, the second most common answer was option 3, then option 4, and finally 1.
Answer 1 is incorrect. 9.71% chose this answer, “Endogenous insulin titer.” This is a juicy answer. Evaluating endogenous insulin production is helpful since it reflects how much insulin the pancreas is secreting. However, it does not reveal if the beta cell loss is due to an immune-mediated response.
Answer 2 is correct. 57.56% of you chose this answer, “Glutamic acid decarboxylase (GAD)”, YES, this is the best answer. If the autoimmune blood test GAD comes back positive, it verifies that the pancreas is being destroyed through an immune-mediated attack of the beta cells. Autoantibodies against GAD are found in 80% of people with type 1 diabetes at clinical presentation.
Answer 3 is incorrect. 22.88% of respondents chose this answer, “Beta cells autoantibodies.” Another juicy answer that is very tempting. However, there is no blood test with this name. The three common antibodies tested are Islet Cell Autoantibodies (ICA), Insulin Autoantibodies (IAA), and Glutamic Acid Decarboxylase (GAD).
Finally, Answer 4 is incorrect. 9.85% chose this answer, “Langerhan’s antibody titer.” Another juicy answer that is very tempting. However, there is no blood test with this name. The three common antibodies tested are Islet Cell Autoantibodies (ICA), Insulin Autoantibodies (IAA), and Glutamic Acid Decarboxylase (GAD).
This bundle includes our CDCES Online Prep Bundle plus the ADCES Review Guide.
The online bundle includes Level 1, Level 2, and Level 3 (Boot Camp), plus two bonus courses. The ADCES Review Guide offers over 480+ practice questions and is a fantastic independent study tool and comprehensive resource for the Diabetes Care and Education Specialist Exam.
Read More: What is a CDCES? First awarded in 1986, as Certified Diabetes Educator (CDE) credential and in 2020 with a new name: Certified Diabetes Care and Education Specialist (CDCES) to more accurately reflect the specialty. CDCES has become a standard of excellence for the delivery of quality diabetes education. Those who hold this certification are known to possess comprehensive knowledge of and experience in diabetes prevention, management, and prediabetes. “Becoming a Certified Diabetes Care and Education Specialist (CDCES) is one of the best professional and personal decisions I have ever made.” – Coach Beverly Thomassian, RN, MPH, CDCES, BC-ADM 
Read More: 3 Reasons to Become a CDCES “The best part of becoming a CDCES is working with my colleagues and people living with diabetes. As diabetes educators, we hear compelling and beautiful life stories. I am astounded by the barriers they face and inspired by their adaptability, problem-solving skills, and resilience.” Reason 1: CDCES is a widely recognized certification by employers and health care professionals throughout the U.S. This credential demonstrates a specialized and in-depth knowledge in the prevention and treatment of individuals living with pre-diabetes and diabetes. Reason 2: Currently, 10% of people in the U.S. have diabetes and another 35% have pre-diabetes which means 45% of Americans are running around with elevated blood glucose levels. Given this epidemic, there will be plenty of future job opportunities. Reason 3: Having my CDCES along with my nursing degree, has opened many doors of opportunity; from working as an inpatient Diabetes Nurse Specialist in a hospital to working as a Manager of Diabetes Education in the outpatient setting to starting my own consulting company.
Sign up for Diabetes Blog Bytes – we post one daily Blog Byte from Monday to Friday. And of course, Tuesday is our Question of the Week. It’s Informative and FREE! Sign up below!
The use of DES products does not guarantee the successful passage of the CDCES exam. CBDCE does not endorse any preparatory or review materials for the CDCES exam, except for those published by CBDCE.