Ready to get certified?
Free CDCES Coach App

Subscribe
eNewsletter
Download
Free Med Pocket Cards
How Not Winning Motivated Me to Write A Book

Several years ago, I was nominated for Diabetes Educator of the Year. Being put forward by colleagues I deeply respected and admired was profoundly meaningful—and, honestly, a little overwhelming.
The nomination felt like recognition of decades of clinical work, teaching, mentoring, and advocacy for person-centered diabetes care. After submitting the detailed application, I allowed myself to feel hopeful. I imagined sharing my philosophy of judgment-free diabetes care with audiences across the country, offering a message of healing for both healthcare professionals and the people they serve. I even choreographed my walk-up dance in my head, ready to hit the ground running.
Then the email arrived from the board: I hadn’t been selected.
I won’t pretend it didn’t sting. I was devastated. Awards matter because they symbolize recognition; they affirm that your voice has value. When I wasn’t chosen, I found myself sitting with a familiar response that many healthcare professionals have experienced: a complicated mix of disappointment, sharp self-doubt, and the well-worn instinct to minimize the hurt and simply move on.
But once the initial ache softened, something important came into focus. I realized that while awards can amplify a message and provide a platform for it, they are not the source of the message itself. And my message was still burning—undiminished—inside me.
The Message Wouldn’t Let Me Go
For years, I had been witnessing something under the surface of diabetes care and, more broadly, of healthcare. Earnest and compassionate clinicians were giving their all to provide the best care, but felt they weren’t breaking through or reaching people in ways that led to significant change. Many were questioning their worth, their effectiveness, and even their decision to enter healthcare at all.
I heard it in hallway conferences. In mentoring meetings. In calm moments after lectures when someone would come up to me and say, “I thought it was just me.”
I knew then that the story I was burning to share couldn’t be reduced to a title or an award category. The message I was holding wasn’t just about diabetes education and achieving an A1C of less than 7%. It was about the emotional gift of caring—and the healing strength of connection.
Choosing Impact Over Recognition
Not winning that award forced a reckoning moment: How could I share my message on a bigger stage?
The answer surprised me with its clarity. Write a book.
I wrote Healing through Connection for Healthcare Professionals because this story matters, award or no award.
The lived experiences and emotional well-being of healthcare professionals matter. You can make a bigger impact in the care you provide by taking inventory of your inner dialogue and beliefs.
Working with people living with diabetes can be filled with connection, joy, and revitalization. By leaving judgment at the door and accepting each other as we are – messy, complicated, and beautiful- you can deepen your connection. The unvoiced grief, the unresolved trauma, the silent resilience, can all have a voice at the table. As a healthcare professional, you deserve healing too.
From Disappointment to Direction
Not winning hasn’t stopped me from sharing my message; it motivated me to find a different way to share it.
It pushed me to write honestly about:
- How your personal history walks into the exam room with you.
- How to create a meaningful connection with the people in our care and provide healing that flows both ways.
- How to revitalize your creativity and give yourself permission for self-care.
This book is not a rebuttal to an award committee.
It’s a love letter to healthcare professionals who keep showing up even when recognition is scarce.
The Real Win
Today, when a nurse, pharmacist, dietitian, or physician tells me, “This book made me feel less alone,” I know I chose the right path.
I didn’t win an award, but I found my voice and shared my authentic life story in my book. This book is my commitment transparency with the hopes that it gives you permission to share your truth.
I wrote Healing through Connection so that other healthcare professionals can share their story and create a healing space for themselves and the people in their care.
Because in the end, the greatest legacy is knowing that your message touched the lives of your community and created space for more compassion, for us and those in our care.
Healing through Connection for Healthcare Professionals
Zoom Celebration Gathering

Join Coach Beverly for a Book Celebration on February 20th at 11:30am PST.
Coach Beverly is thrilled to invite you to join this celebration of completing her book and finally getting the Audible and Kindle version up on Amazon.
We will be discussing why this book matters now more than ever. She will share real stories from her clinical practice and ask you to share yours.
Coach Bev will discuss the process involved in writing this book and how she found her voice. We will wrap up with a question-and-answer session. We hope you can join us.
Invite your friends and colleagues too!
Question of the Week | What Not to Say to Overwhelmed Individual
Maria, a 52‑year‑old woman with type 2 diabetes for 8 years, attends a follow‑up visit. Her A1C has risen from 7.8% to 9.2% over the past year. She reports feeling “overwhelmed” and says she didn’t want to start the medication her clinician recommended at the last visit. She explains, “I’m scared of side effects, and I feel like needing medication means I failed.”
Which of the following responses is the least appropriate (i.e., the WRONG thing to say) to Maria?
- “It sounds like you’re feeling overwhelmed. Can you tell me more about what worries you most about starting this medication?”
- “Many people feel this way. Let’s look at your options together so you can make a choice that works for you.”
- “I understand that this is challenging and overwhelming. However, if you don’t start this medication, you are choosing to risk complications like kidney disease or blindness.”
- “It’s completely understandable to have concerns. Would it help if we reviewed what the medication does, talk about the pro’s and the con’s, and about what alternatives exist?”
Learn More From The Experts:
William H. Polonsky, PhD, CDCES, and Susan Guzman, PhD
ENGAGING THE DISENGAGED | Live in San Diego at Marina Village
April 18th, 2026 from 9 AM to 4 PM PST!

In this course, William H. Polonsky, PhD, CDCES, and Susan Guzman, PhD, examine the powerful role of psychosocial factors in diabetes self-management. Through innovative strategies, participants will learn how to recognize and address common barriers to effective self-care and cardiometabolic medication initiation and maintenance, while fostering respectful, stigma-free clinical encounters.
Through a collaborative and person-centered approach, the course emphasizes communication strategies that enhance motivation, build confidence, and reinforce the value of self-management. Participants will develop skills in diabetes-focused action planning, addressing medication hesitancy, and providing ongoing support and resources to sustain behavior change over time. The goal is to help clinicians make diabetes care more doable, meaningful, and effective for people living with diabetes.
February 2026 eNews
Featured Articles & Announcements ___________________________ |
- Spreading the Love Sale | Ends Feb 16th
- Why Not Winning Motivated Me to Write a Book
- Professional Practice Groups in the Digital Age
- High Five for Fiber
- Diabetes Tech and Distress
- Question of the Week
- Scholarships for Diabetes Virtual DiabetesEd Conference- Due Feb 15th
Webinars & Programs
___________________________
February is the Month of Love — and We’re Embracing It
Greetings, healthcare colleagues!
As healthcare professionals, we’re often invited into the most tender moments of people’s lives. In these moments, you may notice your heart swell with compassion, sorrow, or deep gratitude. While this emotional labor is rarely acknowledged, I want you to know: I see it. I hear it.
We recognize the love and care you give each day. Whether it’s an after-hours check-in, helping with food access, volunteering at a community event, or offering a much-needed hug.
This February, let’s take a moment to honor you and the quiet heroism of showing up again and again with an open heart. In celebration, we are kicking off our “Spreading the Love Sale” starting today!
In this newsletter issue, I share how not being selected for a diabetes educator award led me to a deeper realization and lit a fire to share my message by writing a book.
We also highlight the power of professional connections and the importance of membership in shaping a healthcare future that reflects our values and vision. A special thanks to Sarah Hormachea, RD, MS, CDCES, BC-ADM for her meaningful insights and guest article contribution.
In celebration of fiber, don’t miss nutrition expert Christine Craig’s article featuring the unsung benefits of fiber plus a high five list.
A tech-focused feature from Dr. Beattie explores how technology and diabetes distress can be linked, along with tools to address it.
You are the heartbeat of health care! Here’s to leading with love this month and every month.
With hearts full of gratitude,
Coach Beverly, Bryanna, Astraea & Katarina
Spreading the Love Sale | 15% Off
Use Code “LOVE15“ at Checkout!

Prepare For Your CDCES Exam
Get Exam-Ready With Confidence
Basic & e-Deluxe CDCES Boot Camp Bundle includes:
- Levels 1, 2, and 3 of our Online University
- 30+ expert-led courses
- 50 CE/CPEUs
- 400+ online practice questions
- Handouts, podcast, video and one year access—all in one streamlined platform.
CDCES Boot Camp | 50+ CEs
Starting: $449 | Sale Price: $381.65
Use the Code “LOVE15” for 15% Off at Checkout!
Our CDCES Boot Camp Online Prep Bundle is a comprehensive, high-impact program built specifically for healthcare professionals preparing for the Certified Diabetes Care and Education Specialist (CDCES) exam.
✔ Earn CE/CPE credit through AMA PRA Category 1 Credits™, ACPE, ANCC, and CDR. For more information on accreditation, visit the registration page on our Online Store and click the “Accreditation” tab.
✔ Learn at your pace with expert-led, exam-focused content
✔ Everything you need—organized, practical, and in one place
✔ Perfect for self-directed learners who want complete, person-centered content for clinical practice and exam prep.
✔ Build knowledge, sharpen test-taking skills, and prepare with confidence—on your schedule.
Focused. Flexible. Proven.
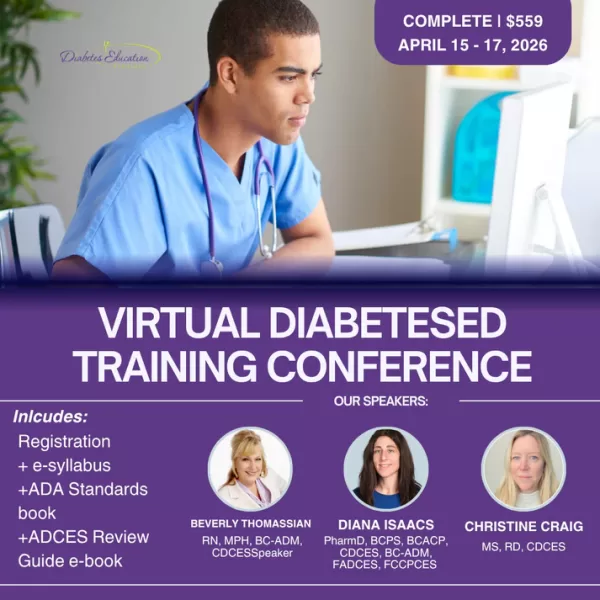
Level-Up With Our Virtual DiabetesEd Training
April 15th-17th, 2026
Registration Fee includes
- 🎤 3 days of engaging, expert-led education
- 19.5 CEs for Pharmacists, Nurses, RDN’s
- 📘 100-page electronic syllabus +
- 🎓 12 FREE bonus online courses ($375 value) to boost your prep
Starting: $429 | Sale Price: $364.65
Use the Code “LOVE15“ for 15% Off at Checkout!
Gain fresh insights, practical tools, and a deeper understanding of the latest in person-centered diabetes care. Our expert team brings the ADA Standards of Care to life—covering medications, behavior change, technology, and more!
If you’re renewing your CDCES or BC-ADM certification this live conference, paired with a handful of free bonus courses, serves as the ideal renewal companion!
Registration Options at a Glance
- 📜 Essentials: Includes registration and electronic syllabus.
- 🌟 Deluxe: Includes registration, electronic syllabus, and the ADA Standards Book for deeper study.
- 🏆 Complete: Best value! Includes everything listed above, plus the ADCES Review Guide of over 400 practice questions for exam prep.
- 🧑🎓Content counts toward ADA Standards requirements for CDCES Renewal.
- 🩺Course credits through AMA PRA Category 1 Credits™, ACPE, ANCC, and CDR!
Level 2 ADA Standards Courses | Take 15% OFF
Course credits through AMA PRA Category 1 Credits™, ACPE, ANCC, and CDR!
Upcoming FREE Certification Webinars

Feb. 19th, 2026 at 11:30 AM PST
Join this FREE, pharmacist-focused webinar Co-led by Diana Isaacs, PharmD, BCPS, BC-ADM, BCACP, CDCES, FADCES, FCCP, Endocrinology Clinical Pharmacy Specialist and Coach Beverly Thomassian, RN, MPH, CDCES, BC-ADM.
Leave with a practical roadmap for achieving Certification Diabetes Care and Education Specialist (CDCES) or Board Certification in Advanced Diabetes Management (BC-ADM).
March 31st, 2026 at 11:30 AM PST
Taking the CDCES Exam in the next 6 months? Register for our Step 2, “Prep to Take the CDCES Exam” FREE Webinar today!
Coach Beverly will review examination process, sample test questions, and the reasoning behind choosing the BEST answers. Gain valuable insights on the exam content and boost your knowledge and test taking confidence. Hope to see you there.
Rationale of the Week | Best Response for Facilitating Positive Health Behavior Change?
For last week’s practice question, we quizzed participants on recommendations for facilitating positive health behavior change, according to 2026 ADA Standards. 81.75% of respondents chose the best answer. We want to clarify and share this important information, so you can pass it on to people living with diabetes and your colleagues, plus prepare for exam success!
Before we start though, if you don’t want any spoilers and haven’t tried the question yet, you can answer it below: Answer Question

KC has type 2 diabetes, diagnosed 5 years ago. They report low physical activity, frequent sugar-sweetened beverage intake, and high stress related to work. Last A1c was 8.2%. KC reports previous advice to “exercise more and drink less soda,” but reports making minimal changes. They express interest in improving health but feels overwhelmed by where to start.
Which of the following responses best aligns with the 2026 ADA Standards of Care recommendations for facilitating positive health behavior change?
- Advise KC to stop sugary drinks and record physical activity minutes daily.
- Ask KC, “What makes improving your health important to you right now?”
- Focus the visit on intensifying glucose lowering medications first and revisit lifestyle changes at the next appointment.
- Recommend KC find social support for activity at the local gym and work with KC to set goals to avoid sugar-sweetened beverages.

Getting to the Best Answer
Answer A is incorrect: 2.38% chose this answer, “Advise KC to stop sugary drinks and record physical activity minutes daily.” Although the Standards of Care do recommend avoiding sugar-beverage consumption and increased activity, this answer is prescriptive and not collaborative. Simply telling the patient what to do without assessing motivation or barriers does not align with ADA recommendations for patient-centered behavior change.
Answer B is correct: 81.75% chose this answer, “Ask KC, “What makes improving your health important to you right now?”” This question is an example of a response using the strategy of motivational interviewing (MI). MI is a patient-centered counseling method that explores readiness, addresses ambivalence, helps patients identify barriers to behavior change and encourages confidence while setting goals. The 2026 ADA Standards of Care recommend using MI, along with other strategies, to help individuals with diabetes adopt sustainable lifestyle behaviors, including diet, physical activity, and stress management.
Answer C is incorrect: 3.57% chose this answer, “Focus the visit on intensifying glucose lowering medications first and revisit lifestyle changes at the next appointment.” While medication intensification may be a first step and necessary approach to support KC is their diabetes management, it fails to first address KC’s goals and desires. In addition, the 2026 ADA Standards of Care emphasize integrating behavior change support alongside pharmacologic therapy.
Answer D is incorrect: 12.3% chose this answer, “Recommend KC find social support for activity at the local gym and work with KC to set goals to avoid sugar-sweetened beverages.” While this option does consider strategies of social support and goal-setting it lacks assessment of readiness and barriers and again is a more prescriptive approach vs. collaborative approach.
We hope you appreciate this week’s rationale! Thank you so much for taking the time to answer our Question of the Week and participate in this fun learning activity!
Learn More About 2026 ADA Standards
With Our Level 2 Courses & Spreading the Love Sale!
Spreading the Love Sale
Save 15% on ALL of Our Online Courses
Use the Code "LOVE15" for 15% Off at Checkout!

Sale Ends on February 16th, 2026!
Question of the Week | Which Feature Most Strongly Supports a Diagnosis of HHS Rather Than DKA?
A 32-year-old with newly discovered diabetes is brought to the emergency department with polyuria and lethargy. They have been sleeping more than usual.
Initial labs show:
- Plasma glucose: 680 mg/dL
- Potassium 3.7 mEq/L
- Serum osmolality: 335 mOsm/kg
Based on the following labs, which feature most strongly supports a diagnosis of hyperosmolar hyperglycemic state (HHS) rather than diabetes ketoacidosis (DKA)?
- Markedly elevated plasma glucose
- Absence of significant metabolic acidosis
- Out of range potassium level
- Elevated effective serum osmolality
Learn More About DKA & HHS
With Level 2 | Hyperglycemic Crises (DKA, HHS & EDKA) & Our CDCES Boot Camp!
Rationale of the Week | What Does J.C.’s Family History & Lab Work Reveal?
For last week’s practice question, we quizzed participants on J.C.’s family history and lab work, and what it reveals. 80.92% of respondents chose the best answer. We want to clarify and share this important information, so you can pass it on to people living with diabetes and your colleagues, plus prepare for exam success!
Before we start though, if you don’t want any spoilers and haven’t tried the question yet, you can answer it below: Answer Question

J.C. is a ten-year-old female with a family history of type 1 diabetes. Her 7-year-old brother was diagnosed with type 1 diabetes two years ago. J.C. has no complaints and reports feeling well. She enjoys playing sports, including basketball and soccer. Her current BMI is 22.1 (93rd percentile for age). She denies any polydipsia, polyuria, or polyphagia. Her lab work demonstrates a fasting blood sugar of 71 mg/dL, an A1c of 5.0%, normal kidney function, and normal electrolytes. Her diabetes autoantibody panel shows positive glutamic acid decarboxylase (GAD) and islet antigen 2 (IA-2) antibodies, negative zinc transporter 8 (ZnT8) antibodies, and negative insulin antibodies.
What does her lab work reveal?
- Stage 1 Type 1 diabetes
- Stage 2 Type 1 diabetes
- Stage 3 Type 1 diabetes
- Type 2 diabetes
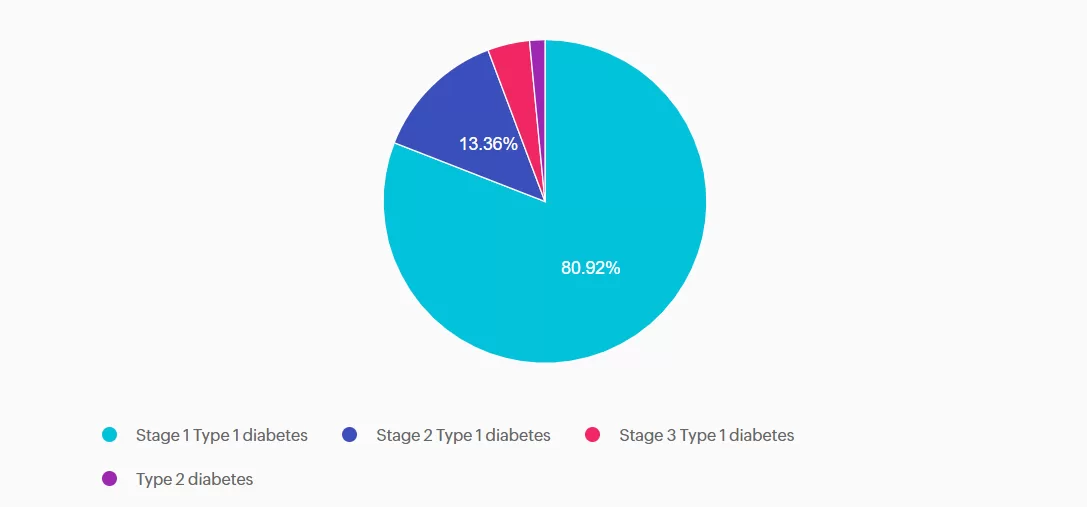
Getting to the Best Answer
Answer A is correct: 80.92% chose this answer, “Stage 1 Type 1 diabetes.” J.C. has stage 1 type 1 diabetes. She has two positive autoantibodies and normoglycemia.
Answer B is incorrect: 13.36% chose this answer, “Stage 2 Type 1 diabetes.” J.C. still has normoglycemia. Stage 2 type 1 diabetes is characterized by positive autoantibodies and dysglycemia (Impaired fasting glucose, Impaired glucose tolerance, or elevated A1c over 5.7% or 10% increase in A1C).
Answer C is incorrect: 4.2% chose this answer, “Stage 3 Type 1 diabetes.” J.C. does not have lab work confirming diabetes by the standard diagnostic criteria, and she is asymptomatic. Stage 3 type 1 diabetes is characterized by overt hyperglycemia and symptoms of diabetes with autoimmunity present.
Answer D is incorrect: 1.53% chose this answer, “Type 2 diabetes.” J.C. does not have type 2 diabetes. She does have a BMI in the overweight category, but she does not have hyperglycemia. She also has positive autoantibodies associated with type 1 diabetes. Type 2 diabetes is not immune-mediated.
We hope you appreciate this week’s rationale! Thank you so much for taking the time to answer our Question of the Week and participate in this fun learning activity!
Learn More About Type 1 Staging & Stds
With Our CDCES Boot Camp Bundle | Includes Level(s) 1-3!
Welcome to our selection of comprehensive CDCES Boot Camp Online Prep Bundles that are specifically designed for healthcare professionals who are studying for the Certified Diabetes Care and Education Specialist (CDCES) exam.
Course credits through AMA PRA Category 1 Credits™, ACPE, ANCC, and CDR!
We offer a selection of prep bundles to meet everyone’s needs! See the descriptions below to review what is included in each option.
CDCES Boot Camp | Basic Exam Prep Bundle: This option is perfect for someone who wants just the Online Courses and materials all in one place, our Online University. This bundle includes Levels 1, 2, and 3 & Toolkits which equates to over 30 courses, 50 CEs/CPEUs, and 400+ online practice questions.
CDCES Boot Camp | e-Deluxe Exam Prep Bundle: This bundle has all of the courses from the Basic Bundle, along with the ADCES Certification Review Guide Practice Questions e-book with 400+ practice questions.
Red Flags for Low Digital Literacy in Diabetes Care

Digital literacy is a key social determinant of health, yet up to one-third of Americans struggle with basic digital literacy skills.¹ In diabetes care, this means many struggle with using, understanding, and applying digital information to improve glycemic control.² As diabetes healthcare providers, how do we know if our clients have low digital literacy? Here are five signs of low digital literacy to watch for in your practice.
1. Difficulty with Technology
- Struggling with using standard technology devices. You may hear: “I have a smartphone, but I don’t know how to use it.”
- Forgetting passwords and needing assistance to log into devices or accounts.
- Not knowing how to download an app on their smartphone or tablet.
2. Device Confusion
- Difficulty understanding how devices connect and share information.
- Confusing diabetes devices. You may hear: “My CGM gives me my insulin.”
- Thinking the insulin pump is “autopilot” and does not enter carbohydrates or meal announcements into the pump.
3. Fear Factor
- Communicating fear of diabetes technology. You may hear: “I just don’t trust those things!” and “What if it gives me the wrong dose?”
- Avoiding eye contact or changing the subject when discussing diabetes technology.
- Expressing worry of becoming overwhelmed with diabetes technology.
4. Technology Comprehension
- Not recognizing or acting on the device alerts and alarms.
- Difficulty interpreting glucose graphs and trend arrows.
- Struggling with troubleshooting the diabetes tech device. You may hear: “I just don’t know why this thing beeps all the time.”
5. Avoidance of Technology
- Shutting down discussion of diabetes technology. You may hear: “I’m too old to learn how to use that.”
- Unwilling to learn how to use the device because the spouse or another family member manages it on their behalf.
- Frequently rescheduling or not coming to training sessions to learn how to use the diabetes device
Improving Digital Literacy
Diabetes healthcare professionals are vital in supporting clients to improve their digital literacy.
✅Acknowledge their fears and concerns. Ask open-ended questions to understand their concerns. During your conversations, address any myths or misconceptions they may have about diabetes technology.
✅ Offer support and assistance with improving their digital literacy skills. Whether it is one-on-one education or in group classes, offer device education sessions tailored to those with low digital literacy.
✅ Increase the frequency of phone calls or in-person check-ins to monitor progress with the diabetes device. Support the client at every step of their learning journey and help them stay accountable for their personal diabetes goals.
References:
- Information Technology & Innovation Foundation. (2021, November 29). Assessing the state of digital skills in the U.S. economy. Retrieved from https://itif.org/publications/2021/11/29/assessing-state-digital-skills-us-economy/
- Huang, E. S., Sinclair, A., Conlin, P. R., Cukierman-Yaffe, T., Hirsch, I. B., Huisingh-Scheetz, M., Kahkoska, A. R., Laffel, L., Lee, A. K., Lee, S., Lipska, K., Meneilly, G., Pandya, N., Peek, M. E., Peters, A., Pratley, R. E., Sherifali, D., Toschi, E., Umpierrez, G., . . . Munshi, M. (2023). The growing role of technology in the care of older adults with diabetes. Diabetes Care, 46(8), 1455. https://pmc.ncbi.nlm.nih.gov/articles/PMC10369127/#B47
Learn More From Our Technology Expert:
Dr. Diana Isaacs
During Our Virtual DiabetesEd Training Conference
April 15th-17th, 2026
Gain fresh insights, practical tools, and a deeper understanding of the latest in person-centered diabetes care. Our expert team brings the ADA Standards of Care to life—covering medications, behavior change, technology, and more!
If you’re preparing for the CDCES or BC-ADM exam, this conference, paired with a handful of free bonus courses, serves as the ideal study companion! Plus, this content counts toward the ADA Standards requirements for CDCES Renewal.
With interactive co-teaching, we keep sessions engaging, relevant, and fun.
Let’s learn and grow together!
Course credits through AMA PRA Category 1 Credits™, ACPE, ANCC, and CDR!
Program Objectives:
Upon completion of this activity, participants should be able to:
- Describe the current ADA Standards for diagnosis, goals, and person-centered diabetes management across the lifespan.
- Demonstrate insulin pattern management and dosing strategies in clinical scenarios.
- Implement timely screening and risk reduction strategies for microvascular and cardiovascular complications.
- Incorporate behavior change techniques and medical nutrition therapy to support people with diabetes self-management and lifestyle adjustment.
Question of the Week | Best Response for Facilitating Positive Health Behavior Change?
KC has type 2 diabetes, diagnosed 5 years ago. They report low physical activity, frequent sugar-sweetened beverage intake, and high stress related to work. Last A1c was 8.2%. KC reports previous advice to “exercise more and drink less soda,” but reports making minimal changes. They express interest in improving health but feels overwhelmed by where to start.
Which of the following responses best aligns with the 2026 ADA Standards of Care recommendations for facilitating positive health behavior change?
- Advise KC to stop sugary drinks and record physical activity minutes daily.
- Ask KC, “What makes improving your health important to you right now?”
- Focus the visit on intensifying glucose lowering medications first and revisit lifestyle changes at the next appointment.
- Recommend KC find social support for activity at the local gym and work with KC to set goals to avoid sugar-sweetened beverages.
Learn More About 2026 ADA Standards
With Our Upcoming Courses & Spreading the Love Sale!
Prepare for the CDCES Exam: Get Ready for Success!
Course credits through AMA PRA Category 1 Credits™, ACPE, ANCC, and CDR!
Get exam-ready with confidence.
Our CDCES Boot Camp Online Prep Bundle is a comprehensive, high-impact program built specifically for healthcare professionals preparing for the Certified Diabetes Care and Education Specialist (CDCES) exam who want to level-up their clinical knowledge and skills.
✔ Learn at your pace with expert-led, exam-focused content
✔ Everything you need—organized, practical, and in one place
✔ Perfect for self-directed learners who want complete, person-centered content for clinical practice and exam prep.
✔ Build knowledge, sharpen test-taking skills, and prepare with confidence—on your schedule.
Focused. Flexible. Proven.
Basic & e-Deluxe CDCES Boot Camp Bundle Includes:
- Levels 1, 2, and 3 of our Online University
- 30+ expert-led courses
- 50 CE/CPEUs
- 400+ online practice questions
- Handouts, podcast, video and one year access—all in one streamlined platform.
Spreading the Love Sale
Save 15% on Certification Boot Camps & Trainings
Use the Code "LOVE15" for 15% Off at Checkout!
CDCES Boot Camp | 50+ CEs
Starting: $449 | Starting Sale Price: $381.65
BC-ADM Boot Camp | 50+ CEs
Starting: $459 | Starting Sale Price: $390.15
Dual-Cert Boot Camp | 60+ CEs
Starting: $519 | Starting Sale Price: $441.15
Virtual Training | 30+ CEs
Starting: $429 | Starting Sale Price: $364.65
Sale Ends on February 16th, 2026!