
Ready to get certified?
Free CDCES Coach App

Subscribe
eNewsletter
Download
Free Med Pocket Cards
Question of the Week | Based on ADA Standards, what is next med addition?
JR has type 2 diabetes and takes Metformin 1000mg BID and sitagliptin (Januvia), A1C 8.1%. GFR 47, UACR 158mg/g. Recent diagnosis of congestive heart failure. These are the medications their insurance covers.
Of the following medications, which addition would most benefit JR?
- glipizide (Glucotrol)
- pioglitazone (Actos)
- semaglutide (Ozempic)
- dapagliflozin (Farxiga)
Ignite your passion & prepare for Diabetes Certification!
Join our Expert Team at our dynamic Virtual DiabetesEd Training Conference April 16-18th, 2025

Gain fresh insights, practical tools, and a deeper understanding of the latest in person-centered diabetes care. Our expert team brings the ADA Standards of Care to life—covering medications, behavior change, technology, and more! If you’re preparing for the CDCES or BC-ADM exam, this conference—paired with free bonus courses—serves as the ideal study companion!
With interactive co-teaching, we keep sessions engaging, relevant, and fun. Let’s learn and grow together!

Our expert team transforms complex diabetes science into clear, practical insights—keeping it real, engaging, and fun! The faculty includes:
- Diana Isaacs, PharmD, BCPS, BC-ADM, BCACP, CDCES
- Coach Beverly Thomassian, RN, MPH, CDCES, BC-ADM
- Christine Craig, MS, RD, CDCES
- 3 Days: of critical information delivered by passionate speakers in an engaging and fun format!
- 11 Bonus Online Courses: As a course attendee, you automatically receive a bonus online course bundle of 11 online courses valued at over
Rationale of the Week | 2025 ADA Standards: Key Nutrition Behaviors for Individuals with Diabetes
For last week’s practice question, we quizzed participants on. 79% of respondents chose the best answer. We want to clarify and share this important information, so you can pass it on to people living with diabetes and your colleagues, plus prepare for exam success!
Before we start though, if you don’t want any spoilers and haven’t tried the question yet, you can answer it below: Answer Question.
Question:
According to the 2025 ADA Standards of Care, which of the following nutrition behaviors are strongly encouraged for individuals with diabetes?
Answer Choices:
- Incorporate onions, garlic, celery, carrots and other vegetables for a base of homemade
foods. - Use herbs and spices to season foods instead of salt containing preparations.
- Water should be the primary beverage of choice.
- Include family or roommate in meal preparation.
- All of the above
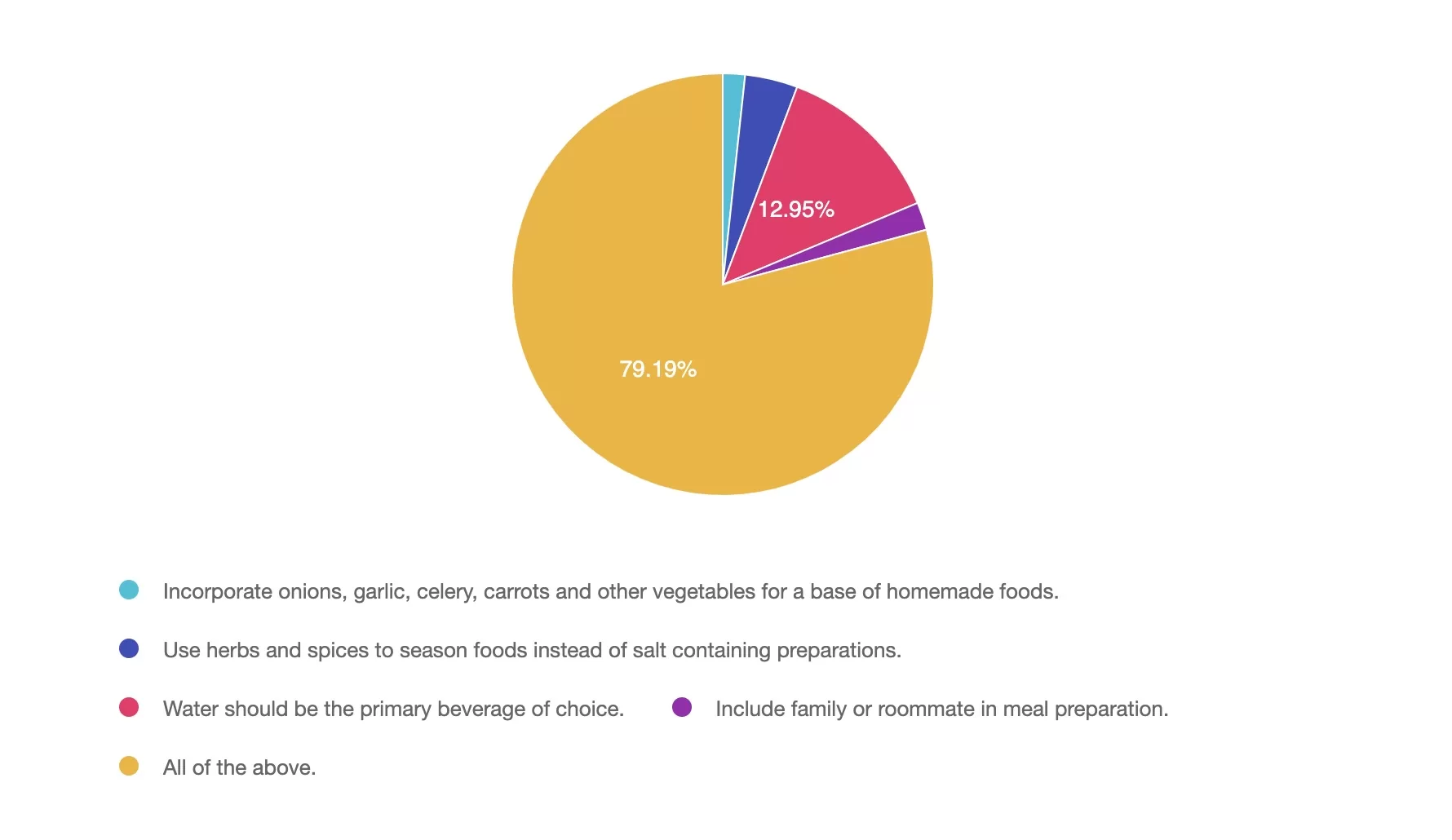
Getting to the Best Answer
Answer 1 is incorrect. 1.7% chose this answer, ” Incorporate onions, garlic, celery, carrots and other vegetables for a base of homemade foods.” Although this answer is true, it is not the best answer. Incorporate onions, garlic, celery, carrots, and other vegetables for a base of homemade foods. These foods can serve as a base to many dishes and incorporates flavor, fiber, vitamins, and minerals while encouraging vegetable consumption.
Answer 2 is incorrect. 4% of you chose this answer, “Use herbs and spices to season foods instead of salt containing preparations.” Although this answer is true, it is not the best answer. 90% of people in the US exceed the daily recommended limits for sodium. Reducing salt intake is important for heart health, managing blood pressure and meeting dietary guidelines. Herbs and spices not only enhance flavor and may provide additional health benefits.
Answer 3 is incorrect. About 12% of respondents chose this, “Water should be the primary beverage of choice.” Although this answer is true, it is not the best answer. The 2025 ADA Standards of Care have emphasized water as the primary beverage of choice. Alternatives to plain water can include no calorie alternatives. Suggestions to add lemon, lime or cucumber to water, choose sparkling no calorie beverages and no-calorie carbonated beverages are also encouraged.
Answer 4 is incorrect. 2% chose this answer, “Include family or roommate in meal preparation.” Although this answer is true, it is not the best answer. Engaging others in meal preparation can create a supportive environment, encourage healthier eating habits, and make cooking more enjoyable. Social support can be especially helpful in managing diabetes long-term.
Answer 5 is correct. 79% chose this answer, “All of the above.” The 2025 ADA Standards of Care encourages all the above nutrition behaviors.
We hope you appreciate this week’s rationale! Thank you so much for taking the time to answer our Question of the Week and participate in this fun learning activity!
Ignite your passion & prepare for Diabetes Certification!
Join our Expert Team at our dynamic Virtual DiabetesEd Training Conference April 16-18th, 2025

Gain fresh insights, practical tools, and a deeper understanding of the latest in person-centered diabetes care. Our expert team brings the ADA Standards of Care to life—covering medications, behavior change, technology, and more! If you’re preparing for the CDCES or BC-ADM exam, this conference—paired with free bonus courses—serves as the ideal study companion!
With interactive co-teaching, we keep sessions engaging, relevant, and fun. Let’s learn and grow together!

Our expert team transforms complex diabetes science into clear, practical insights—keeping it real, engaging, and fun! The faculty includes:
- Diana Isaacs, PharmD, BCPS, BC-ADM, BCACP, CDCES
- Coach Beverly Thomassian, RN, MPH, CDCES, BC-ADM
- Christine Craig, MS, RD, CDCES
- 3 Days: of critical information delivered by passionate speakers in an engaging and fun format!
- 11 Bonus Online Courses: As a course attendee, you automatically receive a bonus online course bundle of 11 online courses valued at over
Question of the Week | What happens when people stop taking GLP /GIPs?
About 30% of people with diabetes started on GLP-1’s stop taking this medication before completing a year of therapy.
According to ADA Standards, what results from sudden discontinuation of GLP-1s /GIP like semaglutide and tirzepatide?
- People maintain their weight loss for at least a year.
- People regain at least one-half of their weight loss within a year.
- People experience decreased nausea and less than 10% weight regain.
- People continue behaviors learned on medication with ongoing weight loss success.
Ignite your passion & prepare for Diabetes Certification!
Join our Expert Team at our dynamic Virtual DiabetesEd Training Conference April 16-18th, 2025

Gain fresh insights, practical tools, and a deeper understanding of the latest in person-centered diabetes care. Our expert team brings the ADA Standards of Care to life—covering medications, behavior change, technology, and more! If you’re preparing for the CDCES or BC-ADM exam, this conference—paired with free bonus courses—serves as the ideal study companion!
With interactive co-teaching, we keep sessions engaging, relevant, and fun. Let’s learn and grow together!

Our expert team transforms complex diabetes science into clear, practical insights—keeping it real, engaging, and fun! The faculty includes:
- Diana Isaacs, PharmD, BCPS, BC-ADM, BCACP, CDCES
- Coach Beverly Thomassian, RN, MPH, CDCES, BC-ADM
- Christine Craig, MS, RD, CDCES
- 3 Days: of critical information delivered by passionate speakers in an engaging and fun format!
- 11 Bonus Online Courses: As a course attendee, you automatically receive a bonus online course bundle of 11 online courses valued at over
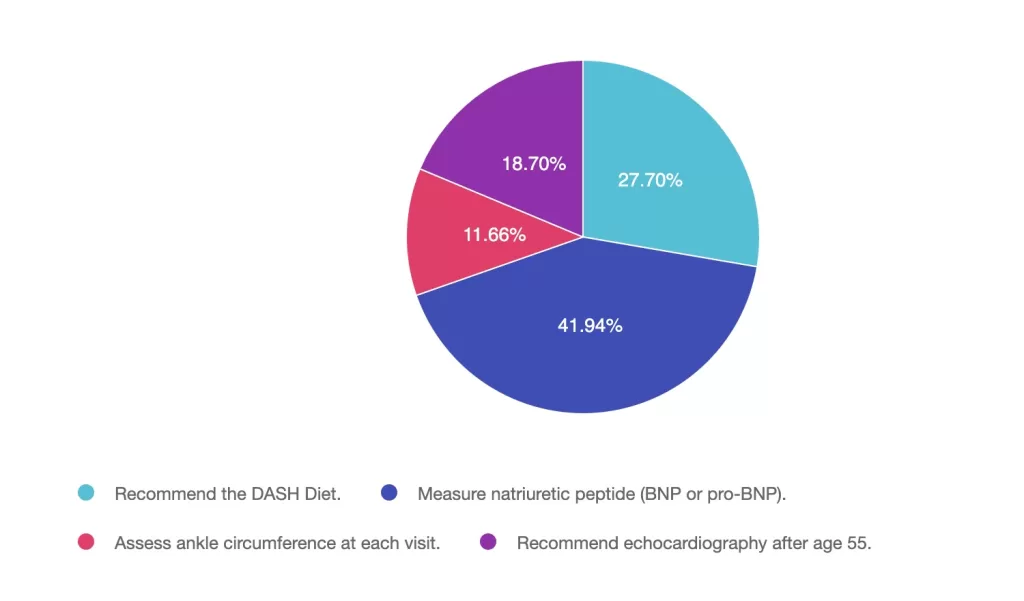
Rationale of the Week | Action needed to prevent heart failure?
For last week’s practice question, we quizzed participants oAction needed to prevent heart failure. 41% of respondents chose the best answer. We want to clarify and share this important information, so you can pass it on to people living with diabetes and your colleagues, plus prepare for exam success!
Before we start though, if you don’t want any spoilers and haven’t tried the question yet, you can answer it below: Answer Question
Question:
Adults with diabetes are at increased risk for the development of asymptomatic or symptomatic heart failure.
According to the ADA 2025 Standards of care, what action is needed to facilitate prevention of heart failure?
Answer Choices:
- Recommend the DASH Diet.
- Measure natriuretic peptide (BNP or pro-BNP).
- Assess ankle circumference at each visit.
- Recommend echocardiography after age 55.
Getting to the Best Answer
Answer 1 is incorrect. 27% chose this juicy answer. “Recommend the DASH Diet.” Although the DASH Diet with lower sodium content is helpful once someone is diagnosed with heart failure, this dietary approach alone won’t prevent heart failure. In order to prevent heart failure, it needs to first be diagnosed to determine best treatment plan.
Answer 2 is correct. 49% of you chose this answer. “Measure natriuretic peptide (BNP or pro-BNP).” YES, Great JOB. According to the ADA Standard on ASCVD, “Adults with diabetes are at increased risk for the development of asymptomatic cardiac structural or functional abnormalities (stage B heart failure) or symptomatic (stage C) heart failure. Consider screening adults with diabetes by measuring a natriuretic peptide (B-type natriuretic peptide [BNP] or N-terminal pro-BNP [NT-proBNP]) to facilitate prevention of stage C heart failure. In asymptomatic individuals with diabetes and abnormal natriuretic peptide levels, echocardiography is recommended to identify stage B heart failure.”
Answer 3 is incorrect. About 11% of respondents chose this. “Assess ankle circumference at each visit.” Although pedal edema and shortness of breath are both indicators of heart failure, the BNP or NT-proBNP lab test is more definitive.
Finally, Answer 4 is incorrect. 18% chose this answer. “Recommend echocardiography after age 55.” According to ADA standards, we would first check the BNP or NT-proBNP lab test. In asymptomatic individuals with diabetes and abnormal natriuretic peptide levels, echocardiography is then recommended to identify stage B heart failure.”
We hope you appreciate this week’s rationale! Thank you so much for taking the time to answer our Question of the Week and participate in this fun learning activity!
Ignite your passion & prepare for Diabetes Certification!
Join our Expert Team at our dynamic Virtual DiabetesEd Training Conference April 16-18th, 2025

Gain fresh insights, practical tools, and a deeper understanding of the latest in person-centered diabetes care. Our expert team brings the ADA Standards of Care to life—covering medications, behavior change, technology, and more! If you’re preparing for the CDCES or BC-ADM exam, this conference—paired with free bonus courses—serves as the ideal study companion!
With interactive co-teaching, we keep sessions engaging, relevant, and fun. Let’s learn and grow together!

Our expert team transforms complex diabetes science into clear, practical insights—keeping it real, engaging, and fun! The faculty includes:
- Diana Isaacs, PharmD, BCPS, BC-ADM, BCACP, CDCES
- Coach Beverly Thomassian, RN, MPH, CDCES, BC-ADM
- Christine Craig, MS, RD, CDCES
- 3 Days: of critical information delivered by passionate speakers in an engaging and fun format!
- 11 Bonus Online Courses: As a course attendee, you automatically receive a bonus online course bundle of 11 online courses valued at over
Question of the Week | 2025 ADA Standards: Key Nutrition Behaviors for Individuals with Diabetes
According to the 2025 ADA Standards of Care, which of the following nutrition behaviors are strongly encouraged for individuals with diabetes?
- Incorporate onions, garlic, celery, carrots and other vegetables for a base of homemade
foods. - Use herbs and spices to season foods instead of salt containing preparations.
- Water should be the primary beverage of choice.
- Include family or roommate in meal preparation.
- All of the above.
Ignite your passion & prepare for Diabetes Certification!
Join our Expert Team at our dynamic Virtual DiabetesEd Training Conference April 16-18th, 2025

Gain fresh insights, practical tools, and a deeper understanding of the latest in person-centered diabetes care. Our expert team brings the ADA Standards of Care to life—covering medications, behavior change, technology, and more! If you’re preparing for the CDCES or BC-ADM exam, this conference—paired with free bonus courses—serves as the ideal study companion!
With interactive co-teaching, we keep sessions engaging, relevant, and fun. Let’s learn and grow together!

Our expert team transforms complex diabetes science into clear, practical insights—keeping it real, engaging, and fun! The faculty includes:
- Diana Isaacs, PharmD, BCPS, BC-ADM, BCACP, CDCES
- Coach Beverly Thomassian, RN, MPH, CDCES, BC-ADM
- Christine Craig, MS, RD, CDCES
- 3 Days: of critical information delivered by passionate speakers in an engaging and fun format!
- 11 Bonus Online Courses: As a course attendee, you automatically receive a bonus online course bundle of 11 online courses valued at over
February 2025 E-Newsletter

Announcements
_________________________
- New “Front-of-Product” Label Proposed
- “Let it Flow” – Semaglutide Approved for CKD
- Marshmallows & Hope: Diabetes Camp
- 14 “Making a Difference” Scholarships – due Feb 24th
- Question of Week
- Rationale of Week
- 20% Off – Spreading the Love Sale Ends Feb 16th!
Upcoming Programs
___________________________
Happy February!
February is all about love, 💙 and that spirit shines brightly in diabetes care and education! We speak from the heart as we advocate for evidence-based care that supports well-being and transforms lives.
In recognition of these daily contributions of diabetes care and education specialists, we are delighted to announce our annual “Spreading the Love” Sale! Enjoy 20% off all our online courses, including program extensions through February 16th.
This month’s newsletter includes exciting information on a new “front-of-package” food labeling proposal that aims to provide more accurate and accessible information for consumers, before adding packaged foods to their carts.
We announce the approval of semaglutide as a first-line agent to protect renal function in people living with chronic kidney disease.
Have you ever considered volunteering at a diabetes camp? After reading this article contributed by a camper and later a diabetes nurse educator, you might be inspired to sign up for a camp near you.
DiabetesEd Services is thrilled to announce an exciting milestone—our first-ever offering of 14 Scholarships for healthcare professionals dedicated to serving under-resourced communities. This initiative is part of our Bridge Program, aimed at mentoring 1,000 new diabetes care professionals over the next ten years.
As always, test your knowledge with our Question and Rationale of the week. We hope to see you at our 3-Day Virtual DiabetesEd Training Conference in April or at a future event!
With love,
Coach Beverly, Bryanna, Tiffany, Christine, & Katarina
Ignite your passion & prepare for Diabetes Certification!
Join our Expert Team at our dynamic Virtual DiabetesEd Training Conference April 16-18th, 2025

Gain fresh insights, practical tools, and a deeper understanding of the latest in person-centered diabetes care. Our expert team brings the ADA Standards of Care to life—covering medications, behavior change, technology, and more! If you’re preparing for the CDCES or BC-ADM exam, this conference—paired with free bonus courses—serves as the ideal study companion!
With interactive co-teaching, we keep sessions engaging, relevant, and fun. Let’s learn and grow together!

Our expert team transforms complex diabetes science into clear, practical insights—keeping it real, engaging, and fun! The faculty includes:
- Diana Isaacs, PharmD, BCPS, BC-ADM, BCACP, CDCES
- Coach Beverly Thomassian, RN, MPH, CDCES, BC-ADM
- Christine Craig, MS, RD, CDCES
- 3 Days: of critical information delivered by passionate speakers in an engaging and fun format!
- 11 Bonus Online Courses: As a course attendee, you automatically receive a bonus online course bundle of 11 online courses valued at over
- e-Syllabus & Resources
Rationale of the Week | ADA 2025: Intensive Prevention for High-Risk Individuals with BMI >35 kg/m2
For last week’s practice question, we quizzed participants on what defines overbasalization according to 2025 ADA Standards? 60% of respondents chose the best answer. We want to clarify and share this important information, so you can pass it on to people living with diabetes and your colleagues, plus prepare for exam success!
Before we start though, if you don’t want any spoilers and haven’t tried the question yet, you can answer it below: Answer Question
Question:
According to ADA 2025 Standards, more intensive preventive approaches should be considered in individuals who are at particularly high risk of progression to diabetes, including individuals with BMI ≥35 kg/m2 who:
Answer Choices:
- Sit more than eight hours a day and have a sedentary lifestyle.
- Have a history of thyroid or celiac disease.
- Consume a diet with high amounts of simple carbohydrates.
- Have fasting plasma glucose of 110–125 or A1C ≥6.0%.
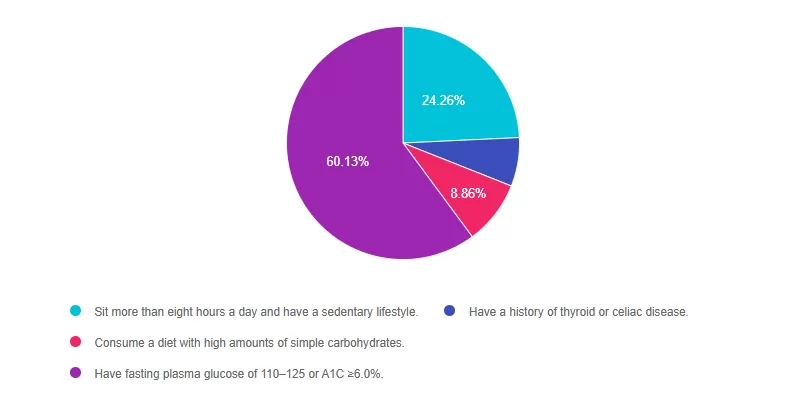
Getting to the Best Answer
Answer 1 is incorrect. 25% chose this answer, “Sit more than eight hours a day and have a sedentary lifestyle”. Although the ADA Standards recommend getting up and moving every half-hour, they don’t specify that eight hours of sitting a day qualifies a person as higher risk to progressing to diabetes.
Answer 2 is incorrect. 7% of you chose this answer “Have a history of thyroid or celiac disease”. These autoimmune conditions are more closely associated with immune mediated type 1 diabetes and do not place a person as higher risk for progression to type 2 diabetes.
Answer 3 is incorrect. About 9% of respondents chose this, “Consume a diet with high amounts of simple carbohydrates.” While eating foods rich in fiber and a variety of nutrients is important to decrease risk of diabetes, the ADA does not state that eating simple carbohydrates puts individuals in a higher risk category of progressing to diabetes.
Finally, Answer 4 is correct 60% chose this answer, “Have fasting plasma glucose of 110–125 or A1C ≥6.0%.” Great job. This is the BEST answer. According to ADA 2025 Standards, “More intensive preventive approaches should be considered in individuals who are at particularly high risk of progression to diabetes, including individuals with BMI ≥35 kg/m2, those at higher glucose levels (e.g., fasting plasma glucose 110–125 mg/dL [6.1–6.9 mmol/L], 2-h post challenge glucose 173–199 mg/dL [9.6–11.0 mmol/L], and A1C ≥6.0% [≥42 mmol/mol]), and individuals with a history of gestational diabetes mellitus.”
We hope you appreciate this week’s rationale! Thank you so much for taking the time to answer our Question of the Week and participate in this fun learning activity!
Ignite your passion & prepare for Diabetes Certification!
Join our Expert Team at our dynamic Virtual DiabetesEd Training Conference April 16-18th, 2025

Gain fresh insights, practical tools, and a deeper understanding of the latest in person-centered diabetes care. Our expert team brings the ADA Standards of Care to life—covering medications, behavior change, technology, and more! If you’re preparing for the CDCES or BC-ADM exam, this conference—paired with free bonus courses—serves as the ideal study companion!
With interactive co-teaching, we keep sessions engaging, relevant, and fun. Let’s learn and grow together!

Our expert team transforms complex diabetes science into clear, practical insights—keeping it real, engaging, and fun! The faculty includes:
- Diana Isaacs, PharmD, BCPS, BC-ADM, BCACP, CDCES
- Coach Beverly Thomassian, RN, MPH, CDCES, BC-ADM
- Christine Craig, MS, RD, CDCES
- 3 Days: of critical information delivered by passionate speakers in an engaging and fun format!
- 11 Bonus Online Courses: As a course attendee, you automatically receive a bonus online course bundle of 11 online courses valued at over
A Life with Type 1 Diabetes: My Camp Journey
by Jeannie Hickey, RN, CDE


Marshmallows and Hope: Bearskin Meadows
In 1965, when I was just 12 years old, my parents dropped me off at Bearskin Meadows, a two-week camp for kids with Type 1 diabetes. It was shortly after I had been diagnosed, and I was still adjusting to my new reality. I remember the daily routines vividly—carrying my cup of urine to the “lab,” lining up for my Regular and NPH injections twice a day, and using meal cards that followed the exchange system for servings.
But even with all that, there were moments of pure joy. I recall playing, singing around the campfire, and yes—roasting marshmallows for s’mores! (A sugary snack at a diabetes camp? Go figure!)
By the time I returned home, I felt much more comfortable with my condition and, more importantly, I felt hopeful. That experience gave me a sense of community and confidence that would shape my relationship with diabetes for years to come.
Fast forward 35 years. Now a Registered Nurse and Certified Diabetes Educator (RN, CDE), I found myself at a “Back to School” conference for parents of children with Type 1 diabetes, hosted by Diabetes Youth Families (DYF). During the event, camp counselors were leading the kids’ activities, and I recognized familiar images from the very same camp I had attended as a child. They invited me to return as a volunteer RN, offering insulin dose adjustments for a group of campers and helping with daily education alongside endocrinologists and other diabetes professionals. (And yes, there were CEUs too!)


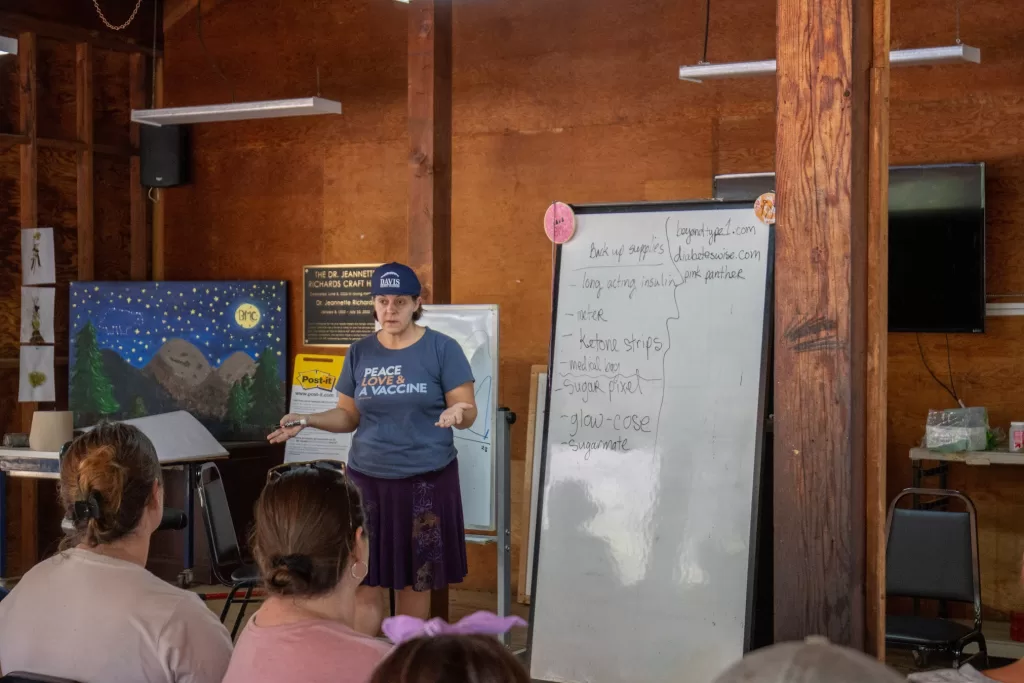
Life Changing Opportunity
That opportunity was life-changing. What started as a one-time volunteer experience quickly turned into a 21-year, part-time summer job. From my initial role as a volunteer, I eventually became the Assistant Medical Director, overseeing the medical care for kids, teens, and families during the two-month camp season. The work I did with Diabetes Youth Families was incredibly rewarding, and I continue to be inspired by the campers and their families each year.
I am thrilled to share my story and encourage you to consider signing up for this unique opportunity of volunteering at T1D camp. You get to learn about and support kids navigating type 1 while diabetes while they are having fun at camp.
Many states have camps, both independent, ADA, or through the Lions. Some offer state CEUs for your volunteer hours and the medical education presented by MDs, other RNs, RDs or Mental Health. DECA – Diabetes Education & Camping Association has a list of accredited camps to consider.
Jeannie Hickey RN, CDE (past Asst Med Dir for Bearskin Meadow Camp through Diabetes Youth Families)
T1D 60 yrs this July!!
If this is an experience you’d like to explore, there are many accredited camps and conferences available. Check out resources like Diabetes Youth Families to find a camp near you and make lasting connections with others living with Type 1 diabetes. Teen Ed Day Sponsorship Packet

What Can Camp Volunteers Expect?
While volunteering at camp your learning objectives are:
- psycho-social issues of living with diabetes
- treatment of hypoglycemia & using Glucagon
- sick day and hyperglycemia treatment
- supporting children in monitoring their blood glucose level and insulin administration
- benefits and challenges of using insulin pumps and sensors
- overall diabetes case management
- diabetes education for a variety of age groups school issues
If new to camp, you will be partnered with a physician or RN until you feel comfortable with the protocol. There will be pump savvy RNs to support & assist your learning. You will not be on your own.
You can also support your Families by learning more about camp and encouraging them to attend as a family, or send their kids (and get a week free from diabetes). See the helpful resources below.
Ignite your passion & prepare for Diabetes Certification!
Join our Expert Team at our dynamic Virtual DiabetesEd Training Conference April 16-18th, 2025

Gain fresh insights, practical tools, and a deeper understanding of the latest in person-centered diabetes care. Our expert team brings the ADA Standards of Care to life—covering medications, behavior change, technology, and more! If you’re preparing for the CDCES or BC-ADM exam, this conference—paired with free bonus courses—serves as the ideal study companion!
With interactive co-teaching, we keep sessions engaging, relevant, and fun. Let’s learn and grow together!

Our expert team transforms complex diabetes science into clear, practical insights—keeping it real, engaging, and fun! The faculty includes:
- Diana Isaacs, PharmD, BCPS, BC-ADM, BCACP, CDCES
- Coach Beverly Thomassian, RN, MPH, CDCES, BC-ADM
- Christine Craig, MS, RD, CDCES
- 3 Days: of critical information delivered by passionate speakers in an engaging and fun format!
- 11 Bonus Online Courses: As a course attendee, you automatically receive a bonus online course bundle of 11 online courses valued at over






