
Subscribe
eNewsletter

Ready to get certified?
Free CDCES Coach App
Download
Free Med Pocket Cards

eNewsletter

Free CDCES Coach App
Free Med Pocket Cards

MK has been living with type 1 diabetes for over 52 years, most recently using an AID system. He views himself as in generally good health “for someone his age” but arrives at this annual visit reporting he recently lost his spouse of more than 46 years. For decades, they shared meals, routines, reminders, and a partnership that often supports confident diabetes self-management. Since her death, MK’s diabetes care has understandably shifted. His eating patterns are now more irregular, medications and boluses occasionally missed, and during the visit conversation, he states, “I should’ve just canceled, I am not doing well in my diabetes.”
Beneath that statement is grief, disorientation from typical patterns and routines, the profound loss of a partner who helped make daily life with diabetes manageable, and possibly more.
It is tempting to jump in and explore with MK how we can help him meet targets and increase his engagement, the way he once did, but grief is a life transition that can change priorities and capacity for self-care. For MJ it altered feelings of support, his social network, motivation, appetite, sleep, and self-efficacy. The American Diabetes Association (ADA) Standards of Care emphasize that diabetes management must be individualized and responsive to individual needs, including psychosocial. Listening and assessing changes in loneliness, social isolation, new goals and expectations, and quality of life may be “what matters most” for this visit. ¹ They also stress that treatment goals and strategies should be modified during significant life transitions, recognizing that the capacity for self-management can change over time.
Person-centered care is our clinical standard of care. Rather than centering the visit on solving assessed problems, it can focus on MK. Sitting with his grief, acknowledging the enormity of loss, and affirming that this is a transition. We can explore what success now means for MK, ensure his safety, and find new points of connection rather than isolation. This visit can support adapting diabetes management to life as it is now, not as it was.
In chronic grief, consideration of concurrent diagnoses such as adjustment disorders, depression, anxiety, lack of social support, and coping mechanisms is important. ² In older adults with depression, an increased risk of suicide had common factors, including recent death of a loved one, social isolation, or the perception of poor health. ³ Using validated screening tools may help identify individuals whose grief is significantly affecting daily functioning and requires additional assessments.
A few examples are the Patient Health Questionnaire-2 or 9 (PHQ-2 or PHQ-9) for depression, the Generalized Anxiety Disorder 7-item scale (GAD-7) for anxiety, and for emotional burden related to living with and managing diabetes, the Problem Areas in Diabetes Scale (PAID), and/or the Diabetes Distress Scale (DDS). 4 A recent article in Diabetes Spectrum 3 reported that the Center for Epidemiological Studies Depression Scale (CES-D), per systematic reviews, was found to be the best-supported tool for measuring depressive symptoms in people with diabetes. Positive screening results do not confirm a diagnosis; communication with the medical team to ensure adequate and ongoing interventions is needed. Referrals to behavioral health specialists, grief counseling, or peer and community support groups may also be recommended. As a resource, the American Diabetes Association has a directory of Mental Health Providers who specialize in supporting individuals with diabetes: https://diabetes.org/tools-resources/mental-health-directory.
Diabetes Care and Education Specialists often take care of individuals over time; we don’t just provide medical assessments, but provide care through significant life events such as marriages, retirements, community disasters, illnesses, changes in caregiving roles, and loss. When working with individuals like MK, presence, active listening, supportive engagement, and collaborative care planning may be the most appropriate interventions. By meeting individuals where they are, rather than where they “should” be, the CDCES supports trust, connection, and access to the care they need. In doing so, we uphold the heart of diabetes care: partnering with people through all seasons of their lives.
References:


J.C. is a ten-year-old female with a family history of type 1 diabetes. Her 7-year-old brother was diagnosed with type 1 diabetes two years ago. J.C. has no complaints and reports feeling well. She enjoys playing sports, including basketball and soccer. Her current BMI is 22.1 (93rd percentile for age). She denies any polydipsia, polyuria, or polyphagia. Her lab work demonstrates a fasting blood sugar of 71 mg/dL, an A1c of 5.0%, normal kidney function, and normal electrolytes. Her diabetes autoantibody panel shows positive glutamic acid decarboxylase (GAD) and islet antigen 2 (IA-2) antibodies, negative zinc transporter 8 (ZnT8) antibodies, and negative insulin antibodies.
What does her lab work reveal?
Welcome to our selection of comprehensive CDCES Boot Camp Online Prep Bundles that are specifically designed for healthcare professionals who are studying for the Certified Diabetes Care and Education Specialist (CDCES) exam.
Course credits through AMA PRA Category 1 Credits™, ACPE, ANCC, and CDR!
We offer a selection of prep bundles to meet everyone’s needs! See the descriptions below to review what is included in each option.
CDCES Boot Camp | Basic Exam Prep Bundle: This option is perfect for someone who wants just the Online Courses and materials all in one place, our Online University. This bundle includes Levels 1, 2, and 3 & Toolkits which equates to over 30 courses, 50 CEs/CPEUs, and 400+ online practice questions.
CDCES Boot Camp | e-Deluxe Exam Prep Bundle: This bundle has all of the courses from the Basic Bundle, along with the ADCES Certification Review Guide Practice Questions e-book with 400+ practice questions.

Featured Articles __________________________ |
Today marks Martin Luther King Jr Day, which gives us pause to reflect on his ideals of equality and justice through acts of service and community care.
Our Bridge Scholarship is rooted in these ideals of service and reciprocity. Our Scholar and Mentorship program goes beyond education—it’s about building connections, fostering professional growth, and creating a vibrant community of passionate diabetes care providers.
We are proud to offer 14 “Making a Difference” Scholarship spots for healthcare professionals to attend our Virtual DiabetesEd Training Conference at no cost or a reduced registration fee. If you or a colleague is seeking to achieve diabetes certification and improve the health of your community, you may qualify for this scholarship opportunity.
Two exciting opportunities to help you on your way!
We are deeply grateful to all the mentors and healthcare professionals who are on their journey toward becoming certified diabetes specialists and leaders in diabetes care.
With heartfelt gratitude,
Coach Beverly, Bryanna, Astraea & Katarina
You are invited to join our FREE Test-Taking Success Webinar on January 23rd, 2026, designed specifically for busy healthcare professionals preparing for diabetes certification.
During this webinar, you will have the opportunity to answer and dissect 20 sample exam questions alongside Coach Bev. Learn how to avoid common exam pitfalls and get to the best answer!
This content will boost your confidence and clarity so you can walk into exam day feeling prepared, calm, and in control. Coach Beverly has helped thousands of candidates cross over the finish line to success. She has passed her CDCES exam 7 times and counting.
🎯 Gain Confidence with Proven Strategies —save your spot today.
We are geared up to help grow and mentor future Certified Diabetes Care and Education Specialists (CDCES) to meet the increasing and varied needs of our diabetes community.
We are offering 14 Bridge Scholarships, which cover the registration cost for our “Virtual DiabetesEd Conference” on April 15-17, 2026. This program will provide you with diabetes fundamentals and beyond! Earn 30+ CEs with access to the courses for one year!
Over the next 10 years we are “Building a Bridge” to welcome a thousand new diabetes educators into the field. If you know a healthcare professional seeking a new challenge and eager to pursue a meaningful and rewarding specialty, please invite them to consider becoming a Certified Diabetes Care and Education Specialist (CDCES).
Get exam-ready with confidence. Our CDCES Boot Camp Online Prep Bundle is a comprehensive, high-impact program built specifically for healthcare professionals preparing for the Certified Diabetes Care and Education Specialist (CDCES) exam. ✔ Earn CE/CPE credit through AMA PRA Category 1 Credits™, ACPE, ANCC, and CDR. For more information on accreditation, visit the registration page on our Online Store and click the “Accreditation” tab. ✔ Learn at your pace with expert-led, exam-focused content ✔ Everything you need—organized, practical, and in one place Perfect for self-directed learners who want complete, person-centered content for clinical practice and exam prep. Focused. Flexible. Proven. Build knowledge, sharpen test-taking skills, and prepare with confidence—on your schedule. |
Get ready for Exam Success Starting Today! Sale ends January 26, 2026! |
CDCES Boot Camp Bundle includes:
Levels 1, 2, and 3 of our Online University
30+ expert-led courses
50 CE/CPEUs
400+ online practice questions
Handouts, podcast, video and one year access—all in one streamlined platform.
Take 15% OFF with coupon code Community15.
Sale ends January 26, 2026!
We are geared up to help grow and mentor future Certified Diabetes Care and Education Specialists (CDCES) to meet the increasing and varied needs of our diabetes community.
We are offering 14 Bridge Scholarships, which cover the registration cost for our “Virtual DiabetesEd Conference” on April 15-17, 2026. This program will provide you with diabetes fundamentals and beyond! Earn 30+ CEs with access to the courses for one year!
Over the next 10 years we are “Building a Bridge” to welcome a thousand new diabetes educators into the field. If you know a healthcare professional seeking a new challenge and eager to pursue a meaningful and rewarding specialty, please invite them to consider becoming a Certified Diabetes Care and Education Specialist (CDCES).
Diabetes Education Services is committed to improving equity and access to diabetes training and education for a diverse group of healthcare professionals. We don’t want financial barriers to stop anyone from attending this conference. In appreciation of those who are role models and advocates for practicing the best diabetes care in their communities.
The Bridge Scholarship program is not just about learning—it’s about creating connections, fostering growth and building a community of passionate diabetes care professionals. We are excited to offer this incredible opportunity to those who are committed to advancing their skills and knowledge in diabetes education. Together, we can make a real difference in the lives of those living with diabetes.
These scholarships are awarded to healthcare professionals who provide care and education to under-served communities that lack access to Diabetes Specialists and healthcare resources. Applicants must be in the process of gaining practice hours and planning to take their CDCES Exam within the next 3 years.
Gain fresh insights, practical tools, and a deeper understanding of the latest in person-centered diabetes care. Our expert team brings the ADA Standards of Care to life—covering medications, behavior change, technology, and more!
If you’re preparing for the CDCES or BC-ADM exam, this conference, paired with a handful of free bonus courses, serves as the ideal study companion! Plus, this content counts toward the ADA Standards requirements for CDCES Renewal.
For last week’s practice question, we quizzed participants on CS’s A1C climbing after experiencing distress. 50.55% of respondents chose the best answer. We want to clarify and share this important information, so you can pass it on to people living with diabetes and your colleagues, plus prepare for exam success!
Before we start though, if you don’t want any spoilers and haven’t tried the question yet, you can answer it below: Answer Question

CS is a 42-year-old with type 1 diabetes for just over 18 years. In the past year, their A1C changed from 7.4% to 9.1%, and weight increased by 20 pounds. Review of CGM data suggests missed insulin boluses more than 7 times per week, and discussion with CS reveals missed clinic visits due to feeling “burned out”. They score in the moderate range on the Diabetes Distress Scale.
Based on the ADA 2026 Standards of Care, which of the following is the most appropriate next step?
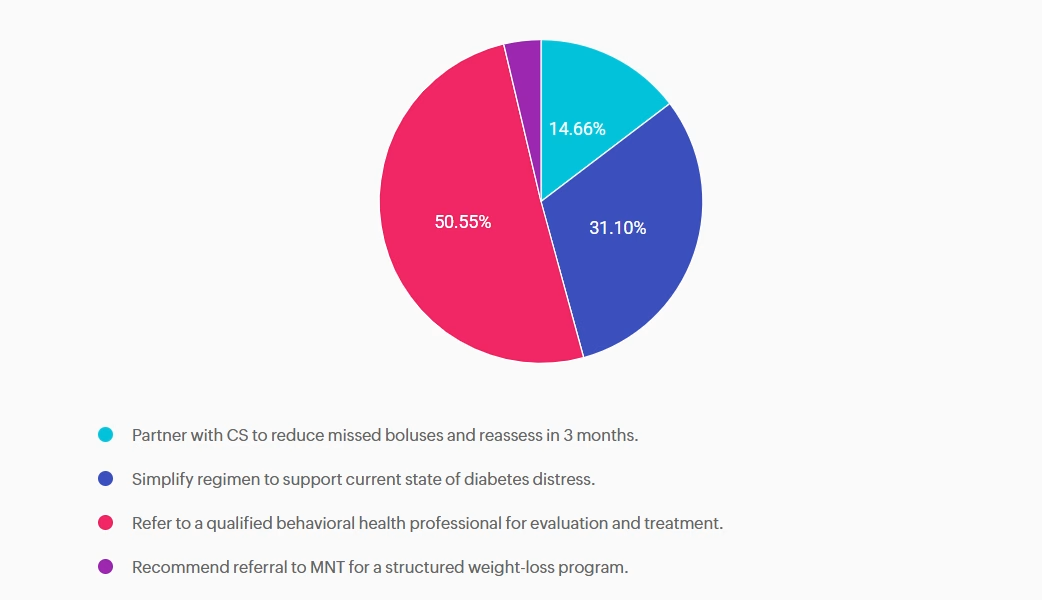
Answer A is incorrect: 14.66% chose this answer, “Partner with CS to reduce missed boluses and reassess in 3 months.” While reducing missed boluses and optimizing insulin therapy are essential to support A1c reduction, this intervention alone does not address the likely underlying psychological barriers to self-management.
Answer B is incorrect: 31.1% chose this answer, “Simplify regimen to support current state of diabetes distress.” While simplifying insulin dosing may be supportive in some cases, without addressing the underlying diabetes distress it is unlikely to achieve sustained improvement.
Answer C is correct: 50.55% chose this answer, “Refer to a qualified behavioral health professional for evaluation and treatment.” The 2026 ADA Standards of Care recommends a referral to a qualified behavioral health professional for evaluation and treatment when diabetes distress, burnout, reduced engagement in diabetes management or other psychosocial factors are impacting self-care and glycemic targets. ¹
Answer D is incorrect: 3.7% chose this answer, “Recommend referral to MNT for a structured weight-loss program.” Focusing solely on weight loss does not address the primary psychosocial barriers and weight gain may be a symptom of underlying behavioral health needs. Evaluation and treatment from a behavioral health provider would be the most appropriate next step.
We hope you appreciate this week’s rationale! Thank you so much for taking the time to answer our Question of the Week and participate in this fun learning activity!

If you’re a busy diabetes healthcare professional, you want tools that help you deliver excellent, evidence-based care—without spending hours digging for information. That’s exactly why we created our Diabetes Cheat Sheet Resource Page, and we’re excited to share that it’s been updated with new additions for 2026.
You can download these free clinical and teaching cheat sheets directly from our website or through the CDCES Coach App. To make your life easier, we’ve reorganized everything by category and alphabetically, so you can quickly find exactly what you need—right when you need it.
The first section focuses on concise, evidence-based clinical summaries drawn from the American Diabetes Association Standards of Care and current research. These resources are ideal for:
The next section includes ready-to-use handouts designed for people living with diabetes. Many are available in both English and Spanish, and several allow you to add your own logo or tailor the content to better serve your population.
A highlight of this section is the new “Keeping Healthy with Diabetes” sheets. These were personally created by Coach Beverly as teaching tools for community classes and for the people she serves in a rural health clinic. They clearly summarize:
Perfect for printing, sharing, and using in real-world conversations.
You’ll also find dedicated sections on:
Whether you’re caring for people with diabetes, teaching others, or preparing for an exam, these updated resources are designed to save you time, reduce overwhelm, and support best-in-class care.

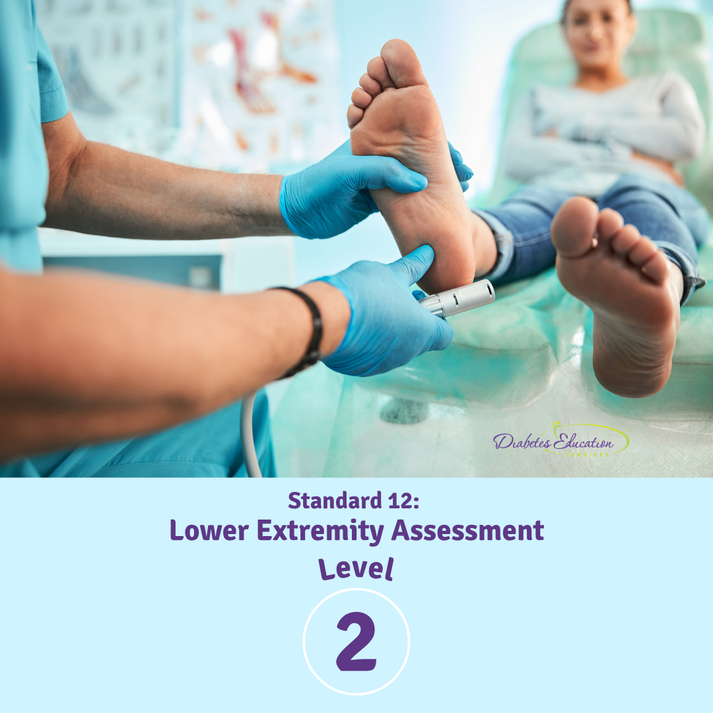
Peripheral Artery Disease (PAD) is significantly underdiagnosed. While PAD affects around 8.5 million Americans and prevalence rises with age (up to 20% over 60), only 10-20% are clinically diagnosed, highlighting a major gap in awareness and screening.
According to the ADA Standards, what needs to be included in the initial screening for PAD?
Featured Articles ___________________________ |
Greetings, wonderful healthcare colleagues!
You are going to love all the updates to our cheat sheets, online university courses, and PocketCards.
Coach Beverly has been excitedly scanning the 2026 ADA Standards to discover updates and advances in diabetes care. She and her team are hustling to integrate these new findings across our platforms, including the CDCES Coach App, handouts, courses, and web content, so that you can access the latest information with confidence.
In our first newsletter of 2026, we are excited to share that we have made significant changes to our Medication PocketCards in the GLP-1/GIP RA section. Now included are the diabetes and weight-loss versions of this popular medication class, with indications for each. You can compare and contrast at a glance. Download your free version and read more below.
Our library of Cheat Sheets is updated and includes a few new additions! These sheets are available on our website and the CDCES Coach App for easy access, with the option to download and share with your colleagues and people living with diabetes alike.
Christine Craig, MS, RD, CDCES, explores her experience with a client who arrived at her office distraught and struggling with the loss of his lifelong partner. Pass the tissues.
Our Tech contributor, Dr. Beattie, provides a summary of red flag statements that may indicate a person is experiencing barriers to effectively using technology in their day-to-day management.
We encourage you to test your knowledge with our Question and Rationale of the Week. January kicks off our Level 1 Fundamental Series, followed by our annual ADA Standards of Care update on January 29th and Level 2 Mastery Course Series in February. We hope to see you there!
Here is to a 2026 filled with self-compassion and moments of awe.
Coach Beverly, Bryanna, Astraea & Katarina