Ramadan & Fasting Considerations for People Living with Diabetes
Ramadan Mubarak… Happy Ramadan.
This evening, Ramadan begins. It is the most important spiritual time for the 1.8 billion Muslims around the world.
In Islam, Ramadan is the month in which the first verses of the Quran, were revealed to the Prophet Muhammad. In observance, many Muslims fast by abstaining from food, drink, smoking, and sex, from pre-sunrise to sunset. This fasting achieves greater “taqwa” or “consciousness to God.”
As Diabetes Care and Education specialists, we have the chance to provide tools for those who fast while keeping diabetes in mind.
The Association for Diabetes Care and Education Specialists (ADCES) put together some helpful handouts to better support people who are fasting and living with diabetes.
Below is the list of resources shared by ADCES
- Fasting and Diabetes web hub
- Fasting with Diabetes Healthcare professionals handout – This handout includes information for potential interventions, potential complications to look out for, nutritional recommendations, and more.
- Ramadan and Diabetes Handout for People Living with Diabetes – English
- Ramadan and Diabetes Handout for People Living with Diabetes – Arabic
To read more about Ramadan, click here.
To take our Question of the Week that considers Type 1 and fasting during Ramadan.
Question of the Week | Why the Post Meal Glucose Spike?
TR can’t figure out why their BG always spikes after breakfast.
How many grams of carb are in the following breakfast? 2 corn tortillas, 2 fried eggs with salsa, ½ cup hashbrowns, and an 8-ounce glass of milk.
- 75 gms
- 57 gms
- 60 gms
- 4 servings
Click Here to Test your Knowledge
Want to learn more about Medical Nutrition Therapy?
You are invited to join our Virtual Conference with our Nutrition expert speaker, Ashley LaBrier, MS, RD, CDCES, who will be providing a half-day presentation on this important topic!

Ashley LaBrier, MS, RD, CDES, is an innovator in the field of diabetes, nutrition, and technology. Ashley is a consultant and the Diabetes Education Program Coordinator at the Salinas Valley Medical Clinic’s Diabetes & Endocrine Center.
Ms. LaBrier is passionate about providing person-centered education to empower those who live with diabetes. Having been diagnosed with type 1 diabetes herself nearly 20 years ago, she combines her professional knowledge with personal experience and understanding.
Virtual DiabetesEd Training Conference

Your team is invited to our Virtual DiabetesEd™ Training Conference! Set your team apart and prepare for diabetes certification!
Join this state-of-the-art conference taught by content experts, Diana Isaacs, PharmD, BCPS, BCACP, BC-ADM, CDCES, Beverly Thomassian RN, MPH, CDCES, BC-ADM, and Ashley LaBrier who are passionate about improving diabetes care.
Group discounts are available!*
All hours earned count toward your CDCES Accreditation Information
Sign up for Diabetes Blog Bytes – we post one daily Blog Byte from Monday to Friday. And of course, Tuesday is our Question of the Week. It’s Informative and FREE! Sign up below!
The use of DES products does not guarantee the successful passage of the CDCES exam. CBDCE does not endorse any preparatory or review materials for the CDCES exam, except for those published by CBDCE.
Rationale of the Week | Is Fast Food the best solution for Food Insecurity?

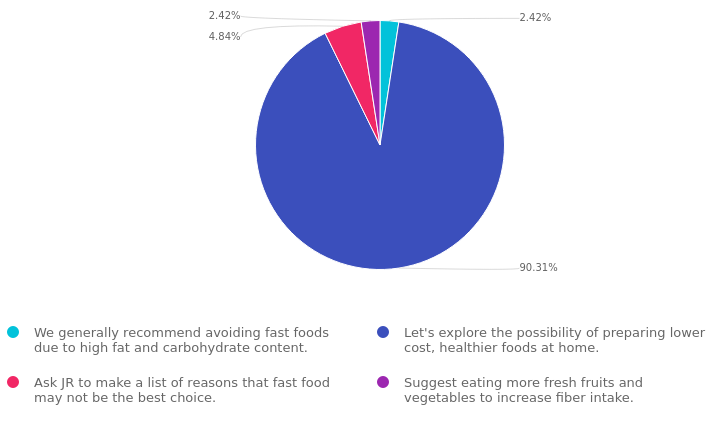
For last week’s practice question, we quizzed participants on if fast food is the best solution for food insecurity. 90% of respondents chose the best answer. We want to clarify and share this important information, so you can pass it on to people living with diabetes and your colleagues, plus prepare for exam success!
Before we start though, if you don’t want any spoilers and haven’t tried the question yet, you can answer it below: Answer Question
Question: Due to the increased cost of groceries, JR tells you all they can afford to eat are fast foods.
As a diabetes care and education specialist, what is the best response?
Answer Choices:
- We generally recommend avoiding fast foods due to high fat and carbohydrate content.
- Let’s explore the possibility of preparing lower-cost, healthier foods at home.
- Ask JR to make a list of reasons that fast food may not be the best choice.
- Suggest eating more fresh fruits and vegetables to increase fiber intake.
Getting to the Best Answer
If you are thinking about taking the certification exam, this practice test question will set you up for success. Test writers anticipate possible answers based on the details in the question. They will wave those “juicy answers” right under your nose. Your job is to weed through the particulars, pluck out the most important elements and choose the BEST answer.
Answer 1 is incorrect. 2.42% chose this answer. “We generally recommend avoiding fast foods due to high fat and carbohydrate content.” While it is true that many fast food options are often high in fat and carbohydrates, we want to honor people choices and situations. This response might be received as critical and could limit the opportunity to collaborate on healthier approaches.
Answer 2 is correct. 90.31% of you chose this answer. “Let’s explore the possibility of preparing lower-cost, healthier foods at home.” GREAT JOB, most chose this BEST answer for good reason. This person-centered approach invites JR to explore lower cost foods that they can prepare at home. It honors JR’s concern over their limited income and invites collaborative problem solving.
Answer 3 is incorrect. 4.48% of respondents chose this. “Ask JR to make a list of reasons that fast food may not be the best choice.” As with the first answer, this response might be received as critical and could limit the opportunity to collaborate on healthier approaches.
Finally, Answer 4 is incorrect. 2.42% chose this answer. “Suggest eating more fresh fruits and vegetables to increase fiber intake.” This answer doesn’t really address the intent of the question and might limit the opportunity to collaborate on problem solving.
We hope you appreciate this week’s rationale! Thank you so much for taking the time to answer our Question of the Week and participate in this fun learning activity!
Want to learn more about Medical Nutrition Therapy?
You are invited to join our Virtual Conference with our Nutrition expert speaker, Ashley LaBrier, MS, RD, CDCES, who will be providing a half-day presentation on this important topic!

Ashley LaBrier, MS, RD, CDES, is an innovator in the field of diabetes, nutrition, and technology. Ashley is a consultant and the Diabetes Education Program Coordinator at the Salinas Valley Medical Clinic’s Diabetes & Endocrine Center.
Ms. LaBrier is passionate about providing person-centered education to empower those who live with diabetes. Having been diagnosed with type 1 diabetes herself nearly 20 years ago, she combines her professional knowledge with personal experience and understanding.
Virtual DiabetesEd Training Conference

Whether you are new to diabetes or a seasoned expert, you’ll benefit from this virtual conference with the latest research plus critical content that you can immediately apply to your clinical practice.
If you are seeking a state-of-the-art review of current diabetes care, this course is for you. Our team has been fine-tuning this course for over fifteen years, and we know what you need. This program can also be a great addition to your CDCES or BC-ADM exam study plan.
Group discounts are available!*
Download Course Flyer | Download Schedule
All hours earned count toward your CDCES Accreditation Information
Sign up for Diabetes Blog Bytes – we post one daily Blog Byte from Monday to Friday. And of course, Tuesday is our Question of the Week. It’s Informative and FREE! Sign up below!
The use of DES products does not guarantee the successful passage of the CDCES exam. CBDCE does not endorse any preparatory or review materials for the CDCES exam, except for those published by CBDCE.
How to Start a Community Fridge
Last month, we launched our very first Community Fridge in our local area!

A few months ago, a group of us got together with the goal of helping to bridge the gaps that lead to food insecurity in our community.
While there are several food banks in our town, there weren’t a lot of options for whole, fresh produce or dairy – focusing on shelf-stable dry goods or meats. We knew other cities had created community fridges and wanted to see if we could offer something similar.
The first step was to find a location; we knew we wanted it to be accessible, but also in an area that could prevent vandalism. We reached out to our local LGBTQ+ center and asked if they had space for a fridge and would be willing to host. After a few conversations, we secured our location.
The second step was to find a fridge. We looked around on Craigslist and found one for free. We got a group of volunteers together to pick up the fridge and drop it off at the LGBTQ+ center.
Lastly, now that we had a fridge and a location, we needed to get the word out. We set up an Instagram and Facebook account, made some flyers, and started sharing posts with our followers.
To ensure there is a rotation of donors throughout the week and that the fridge is cleaned regularly, we created a Calendly to establish a schedule.

During our research, we noticed that other community fridges had best practices and guidelines, such as only donating food you would eat yourself, washing your hands before donating/picking up, and tips for cleaning the fridge. We typed up our own set of guidelines to put on the fridge along with a whiteboard for suggestions/requests for specific foods.
The LGBTQ+ center already has a monthly food bank event, which we decided was the perfect opportunity to introduce the fridge to those who already use the food bank.
The morning of the food bank event, we got together early and made a run to the grocery store. We knew we wanted a variety of fruits, veggies, and dairy, focusing more on items that have a longer shelf life. We decided to also pick up frozen veggies such as spinach, broccoli, and corn, in case someone had access to a freezer and wanted foods that would last a little longer.
We made our way to the LGBTQ+ center and started stocking the fridge. As we were adding in items, person after person came by to pick up food, sharing their ideas for what recipes they were going to make. It was such a joy to hear their inspiration for which produce or dairy matched the meat and dry goods they already got from the food bank.
We are so excited to have this resource available to our community and are looking forward to more people using it.
Written by Bryanna, our Director of Operations & Customer Happiness
FREE Resource Catalog
- Diabetes Cheat Sheets
- Diabetes Blog Bytes
- Medication PocketCards
- Start Your Certification Journey
- CDCES Coach App
- Free Webinars hosted by Coach Beverly
- Question of the Week

See Full Free Resource Catalog
Question of the Week | March 14, 2023
You are teaching about counting fat.
If they ate 2 servings of this Macaroni and Cheese (see label), how many calories would come from total fat?
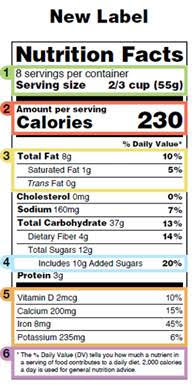
- 16 gms
- 144 kcals
- 460 kcals
- 20%
Click Here to Test your Knowledge
Want to learn more about Medical Nutrition Therapy?
You are invited to join our Virtual Conference with our Nutrition expert speaker, Ashley LaBrier, MS, RD, CDCES, who will be providing a half-day presentation on this important topic!

Ashley LaBrier, MS, RD, CDES, is an innovator in the field of diabetes, nutrition, and technology. Ashley is a consultant and the Diabetes Education Program Coordinator at the Salinas Valley Medical Clinic’s Diabetes & Endocrine Center.
Ms. LaBrier is passionate about providing person-centered education to empower those who live with diabetes. Having been diagnosed with type 1 diabetes herself nearly 20 years ago, she combines her professional knowledge with personal experience and understanding.
Virtual DiabetesEd Training Conference

Whether you are new to diabetes or a seasoned expert, you’ll benefit from this virtual conference with the latest research plus critical content that you can immediately apply to your clinical practice.
If you are seeking a state-of-the-art review of current diabetes care, this course is for you. Our team has been fine-tuning this course for over fifteen years, and we know what you need. This program can also be a great addition to your CDCES or BC-ADM exam study plan.
Group discounts are available!*
Download Course Flyer | Download Schedule
All hours earned count toward your CDCES Accreditation Information
Sign up for Diabetes Blog Bytes – we post one daily Blog Byte from Monday to Friday. And of course, Tuesday is our Question of the Week. It’s Informative and FREE! Sign up below!
The use of DES products does not guarantee the successful passage of the CDCES exam. CBDCE does not endorse any preparatory or review materials for the CDCES exam, except for those published by CBDCE.
March 2023 eNews | Nutrition Month & Strategies to Address Food Insecurity
Happy National Nutrition Month

Join us in celebration of National Nutrition Month with the theme, “Fuel for the Future”.
In this newsletter, we explore food sustainability while providing multiple strategies to address food insecurity. About 20% of people living with diabetes don’t have adequate access to predictable and healthy food. As diabetes care and education specialists, we can take a leadership role in our healthcare communities and on an individual level to make sure people know how to access food and make their dollars stretch when purchasing groceries.
Our first article dives into healthy eating while keeping the environment in mind. We include lots of additional resources to explore and share with your community.
Bryanna, our Director of Operations, details how she helped to create a community refrigerator that offers fresh fruit, veggies, and dairy products for people living with food insecurity. The end result is heartwarming and nourishing.
Coach Beverly provides ideas on maximizing a person’s purchasing power by choosing lower-cost yet super-healthy foods. In addition, this article contains lots of resources on plant-based foods and recipes that are easy to prepare.
We also celebrate Registered Dietitian Nutritionists with a spotlight on our expert Virtual Conference speaker, Ashley LaBrier, MS, RD, CDCES. Did you know that people with diabetes who meet with an RD/RDN have a 0.3 to 2% drop in A1C levels? Dietitians are evidence-based, caring advocates and some of my favorite people.
We hope you enjoy our nutrition-inspired Questions and Rationales of the Week for the entire month of March!
Wishing you a nutritious month,
Coach Beverly and Bryanna
Featured Articles
- National Nutrition Month
- Start a Community Fridge
- Strategies to Address Food Insecurity
- Celebrating Dietitians
- Lilly Insulin Cap of $35
- Question of the Week
- Rationale of the Week
Upcoming Webinars
- Critical Assessment Webinar – March 28th
- Prep CDCES Prep FREE Webinar- March 30th
- Virtual DiabetesEd Training Conference – April 26th
- Upcoming Events – See complete calendar listing
FREE Resource Catalog
- Diabetes Cheat Sheets
- Diabetes Blog Bytes
- Medication PocketCards
- Start Your Certification Journey
- CDCES Coach App
- Free Webinars hosted by Coach Beverly
- Question of the Week

See Full Free Resource Catalog
Sign up for Diabetes Blog Bytes – we post one daily Blog Byte from Monday to Friday. And of course, Tuesday is our Question of the Week. It’s Informative and FREE! Sign up below!
The use of DES products does not guarantee the successful passage of the CDCES exam. CBDCE does not endorse any preparatory or review materials for the CDCES exam, except for those published by CBDCE.
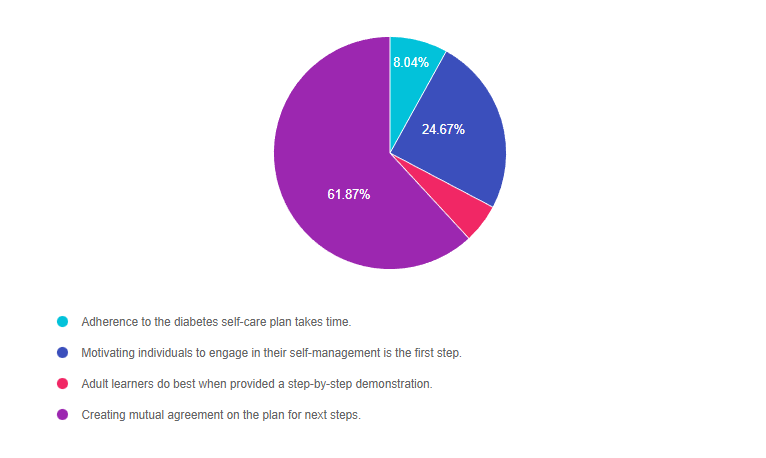
Rationale of the Week | What is Person-Centered Care?

For last week’s practice question, we quizzed participants on person-centered care. 62% of respondents chose the best answer. We want to clarify and share this important information, so you can pass it on to people living with diabetes and your colleagues, plus prepare for exam success!
Before we start though if you don’t want any spoilers and haven’t tried the question yet, you can answer it below: Answer Question
Question: TR is a healthcare professional who provides diabetes care and education support. They are interested in providing more person-centered care to the individuals they serve.
Which of the following statements verifies they are on the right track?
Answer Choices:
- Adherence to the diabetes self-care plan takes time.
- Motivating individuals to engage in their self-management is the first step.
- Adult learners do best when provided a step-by-step demonstration.
- Creating mutual agreement on the plan for next steps.
Getting to the Best Answer
If you are thinking about taking the certification exam, this practice test question will set you up for success. Test writers anticipate possible answers based on the details in the question. They will wave those “juicy answers” right under your nose. Your job is to weed through the particulars, pluck out the most important elements and choose the BEST answer.
Answer 1 is incorrect. 8.04% chose this answer. “Adherence to the diabetes self-care plan takes time.” Under the umbrella of a person-centered care approach, the terms “adherence” and “compliance” are outdated concepts that are no longer used. For example, if we say that TR is adherent, it means that they are following the provider’s instructions instead of being an active participant in care. This person-centered approach engages the individual in the decision-making process and self-care plan.
Answer 2 is incorrect. 24.67% of you chose this answer. “Motivating individuals to engage in their self-management is the first step.” This is a juicy answer that sounds really good. However, it is not a realistic expectation to believe we can motivate people to make changes in their self-management. We can provide coaching and support, but ultimately, the person with diabetes needs to find their own motivation to make slow and steady behavior change. For this reason, this approach is not considered a person-centered approach.
Answer 3 is incorrect. 5.42% of respondents chose this. “Adult learners do best when provided a step-by the-step demonstration.” This answer is partially correct. Adult learners do apply their previous knowledge to the task at hand. However, more importantly than just observing, adult learners need to participate in the learning activity and have “hand’s on” practice to solidify their knowledge.
Finally, Answer 4 is correct. 61.87% chose this answer. “Creating mutual agreement on the plan for next steps.” YES, this is the BEST PERSON-CENTERED ANSWER. This approach invites the person with diabetes to fully participate in determining their needs and goals while making plans for the future in collaboration with the provider.
We hope you appreciate this week’s rationale! Thank you so much for taking the time to answer our Question of the Week and participate in this fun learning activity!
Join us at our
Virtual DiabetesEd Training Conference

Your team is invited to our Virtual DiabetesEd™ Training Conference! Set your team apart and prepare for diabetes certification!
Join this state-of-the-art conference taught by content experts, Diana Isaacs, PharmD, BCPS, BCACP, BC-ADM, CDCES, Beverly Thomassian RN, MPH, CDCES, BC-ADM, and Ashley LaBrier who are passionate about improving diabetes care.
Group discounts are available!*
All hours earned count toward your CDCES Accreditation Information
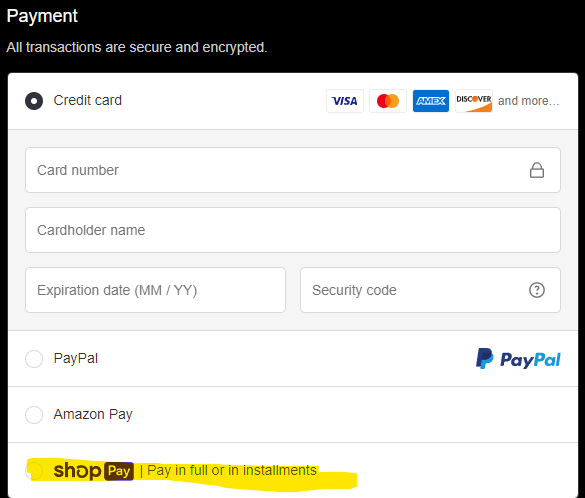
Now introducing payment plans!
Many of you have requested to set up payment plans for your orders and we have found a great solution for this! During checkout, on the payment page, you can now select “Shop Pay” to pay in 3 installments instead of just one payment.
Sign up for Diabetes Blog Bytes – we post one daily Blog Byte from Monday to Friday. And of course, Tuesday is our Question of the Week. It’s Informative and FREE! Sign up below!
The use of DES products does not guarantee the successful passage of the CDCES exam. CBDCE does not endorse any preparator
National Nutrition Month – Tasty Ways to Keep it Sustainable
The Academy of Dietetics and Nutrition is kicking off National Nutrition Month with a new slogan, “Fuel for the Future”.
They are shining a light on considering food consumption through a lens of sustainability. What are some tasty ways to nourish ourselves during every phase of life and protect the environment?
Registered Dietitian Nutritionists are experts in addressing this question. But how can all diabetes care and education specialist help support healthy habits that are sustainable and celebrate the individual’s unique needs?
Strategies to eat with the environment in mind
Plant-Based Meals and Snacks
A great way to get started is to help people learn how to enjoy more plant-based meals and snacks and decrease meat intake. Both the American Diabetes Association and the American Academy of Endocrinologists highly recommend plant-based nutrition for people with diabetes. Not only are plant-based foods packed full of nutrients, protein, and fiber, they generally confer fewer calories and decrease inflammation. Another added bonus is that they have less impact on planetary health and are more sustainable.
Plant-based eating resources including recipes below. Feel free to copy and share!
- Plant-Based Eating Newsletter and Recipes »
- Plant-Based Cooking – Recipes »
- Plant-based diet may benefit patients with diabetes – Smart Brief
- Vegetarian Starter Kit » an easy-to-read and colorful handout for patients interested in learning more about a vegetarian diet. Published by the Physicians Committee for Responsible Medicine.
Sustainable Eating and Decreasing Food Waste
About one-third of all food is tossed into the trash, filling up landfills and increasing methane gas release. Some strategies to decrease waste include finding creative ways to use leftovers rather than tossing them and composting uneaten foods. Encouraging people to buy foods in season and shop locally when possible can make a big impact on the environment while reducing food costs. Another idea is to start a container or backyard garden to grow food at home.
Resources on decreasing food waste and increasing sustainable eating:
- Sustainable Eating article by the Academy of Nutrition and Dietetics
- Food Dates Lead to Waste- Taste Before Tossing
- 5 tips for Sustainable Eating article by Harvard School of Public Health
- Sustainable Eating Resource Hub by Food Print
- Produce from Purchase to Plate – Steps to Reduce Food Waste article by the Academy of Nutrition and Dietetics
- Local Farmer’s Market Finder by Local Harvest – find Community Supported Agriculture farmers in your area.
To stretch dollars, use a grocery list and shop sales when purchasing food. See what foods are at home before purchasing more.
How many times have you returned from shopping, only to discover you already had that bag of carrots tucked away in the back of the refrigerator? But by taking an inventory of what we have and creating a list of what is needed, we can all reduce waste. When shopping, encourage people to start with the outside isles, which generally display healthier foods while avoiding the center and display isles. Incorporating favorite cultural foods into the shopping list and eating foods in various forms including fresh, frozen, canned, and dried, can add to the variety and affordability.
Practice gratitude for your body by giving it the fuel it needs.
Choosing foods that nourish our body and expressing gratitude for the labor and work that went into harvesting and preparing our food, can improve our relationship with food. Making meals at home, by ourselves or with people we live with, can create connections and joy. By learning cooking and meal preparation skills, people have the opportunity to try new foods and enjoy flavors from around the world. Taking time to enjoy our food by mindfully eating and creating long lasting memories with friends and family is a great place to get started on this journey to tasty and sustainable eating.
Happy Nutrition Month everyone and thank you for considering these small changes, which when added up, make a big difference.
Visit the CDR Website for more great ideas and to access a bounty of free resources.
Want to learn more about Medical Nutrition Therapy?
You are invited to join our Virtual Conference with our Nutrition expert speaker, Ashley LaBrier, MS, RD, CDCES, who will be providing a half-day presentation on this important topic!

Ashley LaBrier, MS, RD, CDES, is an innovator in the field of diabetes, nutrition, and technology. Ashley is a consultant and the Diabetes Education Program Coordinator at the Salinas Valley Medical Clinic’s Diabetes & Endocrine Center.
Ms. LaBrier is passionate about providing person-centered education to empower those who live with diabetes. Having been diagnosed with type 1 diabetes herself nearly 20 years ago, she combines her professional knowledge with personal experience and understanding.
Virtual DiabetesEd Training Conference

Whether you are new to diabetes or a seasoned expert, you’ll benefit from this virtual conference with the latest research plus critical content that you can immediately apply to your clinical practice.
If you are seeking a state-of-the-art review of current diabetes care, this course is for you. Our team has been fine-tuning this course for over fifteen years, and we know what you need. This program can also be a great addition to your CDCES or BC-ADM exam study plan.
Group discounts are available!*
Download Course Flyer | Download Schedule
All hours earned count toward your CDCES Accreditation Information
Sign up for Diabetes Blog Bytes – we post one daily Blog Byte from Monday to Friday. And of course, Tuesday is our Question of the Week. It’s Informative and FREE! Sign up below!
The use of DES products does not guarantee the successful passage of the CDCES exam. CBDCE does not endorse any preparatory or review materials for the CDCES exam, except for those published by CBDCE.








