
Subscribe
eNewsletter

Ready to get certified?
Free CDCES Coach App
Download
Free Med Pocket Cards

For last week’s practice question, we quizzed participants on why glucose is spiking after exercise. 80% of respondents chose the best answer. We want to clarify and share this important information, so you can pass it on to people living with diabetes and your colleagues, plus prepare for exam success!
Before we start though, if you don’t want any spoilers and haven’t tried the question yet, you can answer it below: Answer Question
Question:
JR is 42 years old with type 2 diabetes and has worked up to brisk walking for 30 minutes on most days. JR has an A1C of 6.7% and takes an SGLT-2, metformin, and lovastatin along with trying to eat healthfully. JR decided to check blood sugars an hour after exercise and was surprised to see post-exercise blood glucose in the 180’s on two different days. JR asks you why their blood glucose actually rises after exercise.
What is the diabetes specialist’s best response?
Answer Choices:
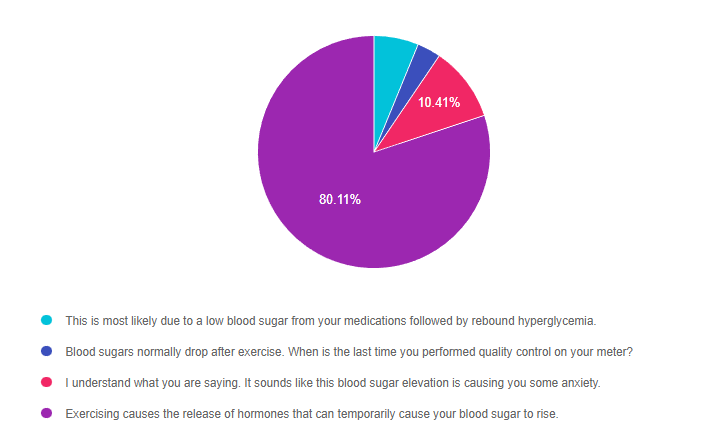
Answer 1 is incorrect. 6.19% chose this answer, “This is most likely due to a low blood sugar from your medications followed by rebound hyperglycemia.” This answer is tempting, but not accurate. Since JR’s only diabetes medication include metformin and a SGLT-2 inhibitor, they are not at risk for low blood sugar. Low blood sugar is only associated with sulfonylureas, meglitinides and insulin therapy.
Answer 2 is incorrect. 3.29% of you chose this answer, “Blood sugars normally drop after exercise. When is the last time you performed quality control on your meter?” In this situation, exercise can decrease hours after exercise, but usually increases immediately after exercise. Which means, JR doesn’t need to perform quality control on their glucose meter, since it is accurately reflecting blood sugar trends.
Answer 3 is incorrect. 10.41% of respondents chose this answer, “I understand what you are saying. It sounds like this blood sugar elevation is causing you some anxiety.” Although, this is a very compassionate response, it does not answer the question JR is asking, “why does my blood sugar go up after exercise?” For this reason, it is tempting, but not the best answer.
Finally, Answer 4 is correct. 80.11% chose this answer, “Exercising causes the release of hormones that can temporarily cause your blood sugar to rise.” YES, most of you chose the best answer. With exercise, counterregulatory or stress hormones are activated, which increases insulin resistance and causes blood glucose levels to temporarily rise to feed hungry muscles. This glucose rise is an expected temporary response and with time, blood sugars get back to baseline. GREAT JOB.
Thank you so much for reading this “Rationale of the Week”.
We also invite you to join our Online Courses for more information (see info below)
Hope you can join our ADA Standards of Care Webinar Update in February.
This bundle is specifically designed for healthcare professionals who want to learn more about diabetes fundamentals for their clinical practice or for those who are studying for the Certified Diabetes Care and Education Specialist (CDCES) exam.
Intended Audience: This library of critical information is designed for individuals or groups of diabetes specialists, including RNs, RDs, Pharmacists, Nurse Practitioners, Clinical Nurse Specialists, Physician Assistants, and other health care providers interested in staying up to date on current practices of care for people with diabetes and preparing for the CDCES Certification Exam.
All hours earned count toward your CDCES Accreditation Information
Join us live on February 2, 2023, at 11:30 am PST for our
This course, updated annually, is an essential review for anyone in the field of diabetes. Join Coach Beverly as she summarizes the 2023 updates to the American Diabetes Association’s Standards of Medical Care in Diabetes and provides critical teaching points and content for healthcare professionals involved in diabetes care and education.
All hours earned count toward your CDCES Accreditation Information
Sign up for Diabetes Blog Bytes – we post one daily Blog Byte from Monday to Friday. And of course, Tuesday is our Question of the Week. It’s Informative and FREE! Sign up below!
The use of DES products does not guarantee the successful passage of the CDCES exam. CBDCE does not endorse any preparatory or review materials for the CDCES exam, except for those published by CBDCE.
In the past, if a person with type 2 diabetes can’t get blood glucose to target on oral meds, the next action would be to add basal insulin. However, the latest guidelines, found in the ADA 2023 Standard 9, encourages providers to consider adding a GLP-1 RA or GIP/GLP-1 RA before writing that prescription for basal insulin.
Diabetes pharmacologic management has dramatically changed over the past few years with the addition of Incretin Mimetics (GLP-1 RA and GIP/GLP-1 RAs) and SGLT2i’s to the medication landscape. The pathways and algorithms have been adjusted to incorporate these newer medication options, which significantly lower glucose without the risk of low blood sugar or weight gain like insulin or sulfonylureas.
GLP-1 RA or GIP/GLP-1 RA versus Insulin Therapy
The truth is, insulin will always lower blood glucose levels, but users may experience the side effects of hypoglycemia and unwanted weight gain. However, for some people, adding insulin is still the next best step. According to the ADA Standard 9, “health care professionals should consider insulin as the first injectable when there is evidence of ongoing catabolism, symptoms of hyperglycemia and when A1C levels >10% or blood glucose levels are 300mg/dL or very high, or a diagnosis of type 1 diabetes is a possibility.”
Insulin can be easily titrated up or down, depending on glucose profile and users can fine tune dosing to match carb intake and other factors. Insulin has been around for over 100 years and has been extensively studied and it’s action and side effects are well understood.
In spite of these benefits, insulin does have some disadvantages. Insulin doesn’t have the same cardiovascular benefits as the GLP-1 RA’s or GIP/GLP-1 RA’s, nor does it contribute to weight loss. Let’s explore some of the benefits of starting with these “Incretin Agonists” before adding insulin therapy.
Benefits of starting Incretin Mimetics; GLP-1 RA’s or GIP/GLP-1 RA’s, before adding insulin therapy
These 2 classes of incretin mimetics lower A1C from 1.6% to 2.4% when used at maximum dose, a significant glucose improvement. In addition, people experience weight loss that ranges from 6% to 13% when on maximum doses. (Please see PocketCard to the right and package inserts for more information)
Data from the CVOTs (Cardiovascular Outcomes Trials) demonstrate that three of the GLP-1 RAs (liraglutide, dulaglutide, semaglutide ) significantly reduce the risk of cardiac death, heart attack and stroke.
Given that the most people living with type 2 diabetes have elevated BMI’s and a high risk for CV disease, it makes sense, when feasible and clinically indicated, to start with GLP-1 RAs or GIP/GLP-1 RAs before initiating insulin therapy. Of course, when selecting GLP-1 RAs or GIP/GLP-1 RAs, we need to consider individual preference, insurance coverage, A1C lowering and weight-lowering effect and frequency of injection. In addition, for those on GLP-1 RA and basal insulin combination, we can consider using a fixed-ratio combination product (iDegLira or iGlarLixi) For more info on dosing and considerations for these two combination products, you can Download FREE Combo Injectable PocketCards.
For a step-by-step approach, please see the 2023 ADA Algorithm for Intensifying Injectable Therapy for People with Type 2 from ADA Standard 9. This algorithm provides a roadmap for health care professionals working to improve glucose levels for those living with type 2 diabetes.
When people with type 2 are not at their glucose targets using oral medications, we are encouraged to thoughtfully consider the next best pharmacologic injectable addition. Given the benefits listed above, the GLP-1RA and GIP/GLP-1 RA therapies may be the best choice for many people living with type 2 diabetes.
Thank you for collaborating with individuals to determine the next best step when needing to add injectables to their management plan. To learn more, you can view our recorded program, Meds for Type 2 Update; New ADA/EASD 2023 Consensus Statement.
We retyped this ADA Standards algorithm in a larger font and on 2 pages, to make it easier to read for studying and so you can post on the wall of your clinical practice.
View ADA 2023 Standard 9, Pharmacological Approaches to Glycemic Treatment here.
RZ is 47 years old with type 2 diabetes and hypertension with a UACR of 199 mg/g. RZ takes metformin 1000 mg BID, plus lisinopril 20mg daily. RZ most recent LDL Cholesterol was 130 mg/dL. The provider writes an order for DASH meal planning education and initiation of atorvastatin 40mg.
Based on the most recent ADA Standards, what is the LDL Cholesterol target for RZ?
Click Here to Test your Knowledge
This course, updated annually, is an essential review for anyone in the field of diabetes. Join Coach Beverly as she summarizes the 2023 updates to the American Diabetes Association’s Standards of Medical Care in Diabetes and provides critical teaching points and content for healthcare professionals involved in diabetes care and education.
Objectives:
Intended Audience: This course is a knowledge-based activity designed for individuals or groups of diabetes professionals, including RNs, RDs, Pharmacists, Nurse Practitioners, Clinical Nurse Specialists, Physician Assistants, and other health care providers interested in staying up to date on current practices of care for people with prediabetes, diabetes and other related conditions.
Don’t worry if you can’t make it live. Your registration guarantees access to the recorded version in the Online University.
All hours earned count toward your CDCES Accreditation Information

Can’t join all the sessions live? No problem. Your registration guarantees you access to the recorded lectures for a full year.
This bundle is specifically designed for healthcare professionals who are studying for the Board Certified in Advanced Diabetes Management (BC-ADM) or the Certified Diabetes Care and Education Specialist (CDCES) certification exam.
Intended Audience: This library of critical information is designed for individuals or groups of diabetes specialists, including RNs, RDs, Pharmacists, Nurse Practitioners, Clinical Nurse Specialists, Physician Assistants, and other health care providers interested in staying up to date on current practices of care for people with diabetes and preparing for the BC-ADM or the CDCES certification Exam.
All hours earned count toward your CDCES Accreditation Information
Sign up for Diabetes Blog Bytes – we post one daily Blog Byte from Monday to Friday. And of course, Tuesday is our Question of the Week. It’s Informative and FREE! Sign up below!
The use of DES products does not guarantee the successful passage of the CDCES exam. CBDCE does not endorse any preparatory or review materials for the CDCES exam, except for those published by CBDCE.
While the celebration of Dr. King is global, its spirit is local. As Dr. King said, “Everyone can be great, because everyone can serve” and there is no better way to honor his legacy than through individual and community service.
As Diabetes Specialists, we honor Dr. King’s words by serving people living with prediabetes and diabetes. We advocate for affordable diabetes care, medications, and access to nutritious foods.
We are fully aware that people with diabetes are more likely to struggle with food insecurity, social and financial inequities and lack adequate resources to pay for medications and diabetes supplies. We know that there is still much work to be done. During these challenging times, I am comforted by Dr. King’s resonant statement “The arc of the moral universe is long, but it bends toward justice.”
On this day of national celebration and service, we thank Dr. King for being a beacon of light and clarity with his call to action that still resonates today.
With Gratitude,
Coach Beverly
Sign up for Diabetes Blog Bytes – . It’s Informative and FREE! Sign up below!
[yikes-mailchimp form=”1″]If you are taking the CDCES or BC-ADM exam in 2023, these new lipid targets for high risk individuals and treatment interventions are important to know.

For all of us who serve people with diabetes, evidence from many trials demonstrated that these more intensive LDL cholesterol targets will save lives and decrease CV disease. By sharing this information with our colleagues and teams, we can be a part of improving outcomes and quality of life.
The following content summarizes the 2023 updated ADA guidelines as outlined in Standard 10 – Cardiovascular Disease and Risk Management.
The guidelines have remained the same for lower risk individuals with diabetes aged 40–75 years without atherosclerotic cardiovascular disease, “Start moderate-intensity statin therapy in addition to lifestyle therapy”. They also are the same for people with diabetes aged 20–39 years with additional atherosclerotic cardiovascular disease risk factors, “Based on individual assessment, initiate statin therapy in addition to lifestyle therapy.”
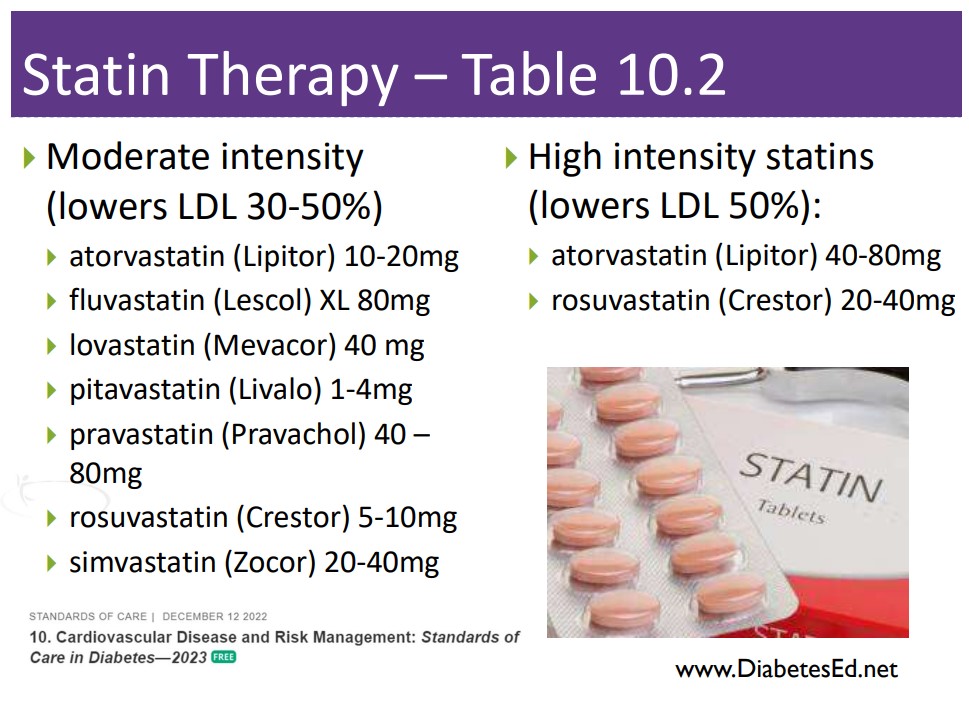
In the category of primary prevention for people with diabetes aged 40–75 at higher cardiovascular risk (LDL >100, HTN, Smoke, CKD, albuminuria, family hx ACSVD), the goals have been intensified.
Secondary Prevention goals have also been intensified.
For people of all ages with diabetes and atherosclerotic cardiovascular disease:
Target LDL cholesterol reduction of 50% or greater from baseline and an LDL cholesterol goal of <55 mg/dL.
Addition of ezetimibe or a PCSK9 inhibitor with proven benefit in this population is recommended if goal is not achieved on maximum tolerated statin therapy.
In 2022, the ADA Standards did not include specific LDL targets for people with diabetes. However, based on recent study results, the committee updated the 2023 guidelines to reflect the latest research findings. To learn more about the study findings, Standard 10 – Cardiovascular Disease and Risk Management.
Keeping track of medications for hypertension and cholesterol can seem daunting. We have put together a Lipid Medication Cheat Sheet along with summary information for each class that is important to know for certification exams and is very useful in clinical practice.
Together, we can improve the quality of life and outcomes for people living with diabetes. Getting LDL cholesterol levels to target is an important interventions to maintain health. Thank you for reading this article and advocating for the best evidence-based care.
This course, updated annually, is an essential review for anyone in the field of diabetes. Join Coach Beverly as she summarizes the 2023 updates to the American Diabetes Association’s Standards of Medical Care in Diabetes and provides critical teaching points and content for healthcare professionals involved in diabetes care and education.
Objectives:
Intended Audience: This course is a knowledge-based activity designed for individuals or groups of diabetes professionals, including RNs, RDs, Pharmacists, Nurse Practitioners, Clinical Nurse Specialists, Physician Assistants, and other health care providers interested in staying up to date on current practices of care for people with prediabetes, diabetes and other related conditions.
Don’t worry if you can’t make it live. Your registration guarantees access to the recorded version in the Online University.
All hours earned count toward your CDCES Accreditation Information
This bundle includes our CDCES Online Prep Bundle (featured above) plus the ADCES Review Guide – 5th Edition-Revised. The online bundle includes Level 1, Level 2, and Level 3 (Boot Camp), plus two bonus courses. The ADCES Review Guide offers over 480+ practice questions and is a fantastic independent study tool and comprehensive resource for the Diabetes Care and Education Specialist Exam.
Enroll now | $499
Our diabetes cheat sheet page is brimming full of useful information for your clinical practice and exam success.
We include a slew of FREE handouts that summarize important topics like; diagnostic criteria, blood pressure and lipid meds, immunization schedule plus patient education handouts, and more.
Updated by Coach Beverly to reflect the 2023 ADA Standards, we invite you to take a look around and enjoy these helpful resources.

Can’t join all the sessions live? No problem. Your registration guarantees you access to the recorded lectures for a full year.
This bundle is specifically designed for healthcare professionals who are studying for the Board Certified in Advanced Diabetes Management (BC-ADM) or the Certified Diabetes Care and Education Specialist (CDCES) certification exam.
Intended Audience: This library of critical information is designed for individuals or groups of diabetes specialists, including RNs, RDs, Pharmacists, Nurse Practitioners, Clinical Nurse Specialists, Physician Assistants, and other health care providers interested in staying up to date on current practices of care for people with diabetes and preparing for the BC-ADM or the CDCES certification Exam.
All hours earned count toward your CDCES Accreditation Information
Sign up for Diabetes Blog Bytes – we post one daily Blog Byte from Monday to Friday. And of course, Tuesday is our Question of the Week. It’s Informative and FREE! Sign up below!
The use of DES products does not guarantee the successful passage of the CDCES exam. CBDCE does not endorse any preparatory or review materials for the CDCES exam, except for those published by CBDCE.

For last week’s practice question, we quizzed participants on who is most at risk of diabetes based on the new ADA Standards. 45% of respondents chose the best answer. We want to clarify and share this important information, so you can pass it on to people living with diabetes and your colleagues, plus prepare for exam success!
Before we start though, if you don’t want any spoilers and haven’t tried the question yet, you can answer it below: Answer Question
Question:
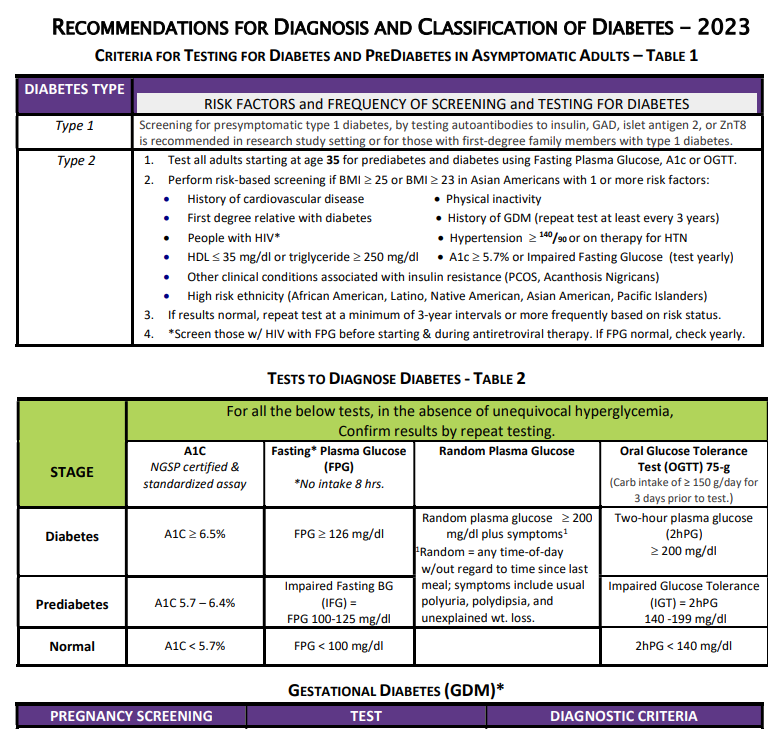
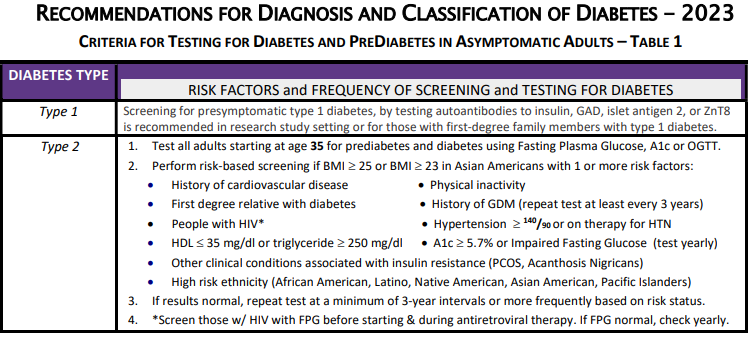
The clinic where JR works as a Diabetes Specialist wants to set up a screening program to identify people with undiagnosed prediabetes or diabetes based on risk status. According to the 2023 ADA Standards of Care, which of the following indicates that an individual is at increased risk of having prediabetes and diabetes and needs further testing?
Answer Choices:
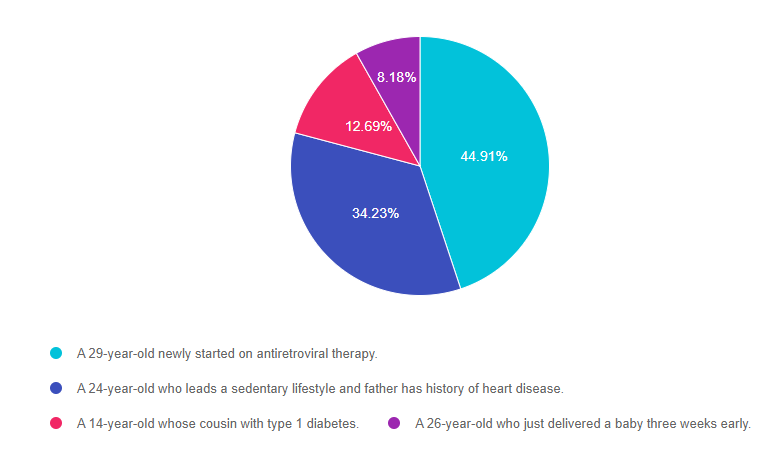
Answer 1 is correct. 44.91% chose the BEST answer, “A 29-year-old newly started on antiretroviral therapy.” GREAT JOB. A potential side effect of antiretroviral therapy, used to treat HIV, is the destruction of beta cells and resultant hyperglycemia. The ADA guidelines recommend screening blood sugars before starting antiretroviral therapy, during treatment and yearly. Of course, it is also important to alert the individual on antiretroviral therapy of the signs of hyperglycemia and ask them to report any signs right away. Please refer to our Diabetes Diagnosis and Screening Cheat Sheet for more information.
Answer 2 is incorrect. 34.23% of you chose this answer, “A 24-year-old who leads a sedentary lifestyle and father has history of heart disease.” Screening for prediabetes or diabetes starts at the age of 35 for everyone or for younger individuals with an elevated BMI and an additional risk factor. Since this person is under the age of 35 and we don’t know their weight, they wouldn’t meet the criteria for a high risk individual based on the information provided and the ADA Guidelines. Please refer to our Diabetes Diagnosis and Screening Cheat Sheet for more information.
Answer 3 is incorrect. 12.69% of respondents chose this answer, “A 14-year-old whose cousin with type 1 diabetes.” The ADA guidelines suggest screening individuals with a first-degree family members with type 1 diabetes. Since cousins aren’t considered first-degree relatives, this is not the best answer. However, JDRF has a Type 1 Screening Resource Page for those who are interested in being screened for type 1 diabetes. Please refer to our Diabetes Diagnosis and Screening Cheat Sheet for more information.
Finally, Answer 4 is incorrect. 8.18% chose this answer, “A 26-year-old who just delivered a baby three weeks early.” This answer is tempting, but does not match the ADA risk factors. A person who had gestational diabetes has a higher risk of future diabetes, but in this answer, there is no indication that the person had GDM or any blood sugar elevations. Delivering a baby early is not associated with increased diabetes risk. Please refer to our Diabetes Diagnosis and Screening Cheat Sheet for more information.
Thank you so much for reading this “Rationale of the Week”.
Please refer to our Diabetes Diagnosis and Screening Cheat Sheet for more information.
We also invite you to join our Online Courses for more information (see info below)
Hope you can join our ADA Standards of Care Webinar Update in February.
This bundle is specifically designed for healthcare professionals who want to learn more about diabetes fundamentals for their clinical practice or for those who are studying for the Certified Diabetes Care and Education Specialist (CDCES) exam.
Intended Audience: This library of critical information is designed for individuals or groups of diabetes specialists, including RNs, RDs, Pharmacists, Nurse Practitioners, Clinical Nurse Specialists, Physician Assistants, and other health care providers interested in staying up to date on current practices of care for people with diabetes and preparing for the CDCES Certification Exam.
All hours earned count toward your CDCES Accreditation Information
Join us live on February 2, 2023, at 11:30 am PST for our
This course, updated annually, is an essential review for anyone in the field of diabetes. Join Coach Beverly as she summarizes the 2023 updates to the American Diabetes Association’s Standards of Medical Care in Diabetes and provides critical teaching points and content for healthcare professionals involved in diabetes care and education.
All hours earned count toward your CDCES Accreditation Information
Sign up for Diabetes Blog Bytes – we post one daily Blog Byte from Monday to Friday. And of course, Tuesday is our Question of the Week. It’s Informative and FREE! Sign up below!
The use of DES products does not guarantee the successful passage of the CDCES exam. CBDCE does not endorse any preparatory or review materials for the CDCES exam, except for those published by CBDCE.
JR is 42 years old with type 2 diabetes and has worked up to brisk walking for 30 minutes on most days. JR has an A1C of 6.7% and takes an SGLT-2, metformin, and lovastatin along with trying to eat healthfully. JR decided to check blood sugars an hour after exercise and was surprised to see post-exercise blood glucose in the 180’s on two different days. JR asks you why their blood glucose actually rises after exercise.
What is the diabetes specialist’s best response?
Click Here to Test your Knowledge
Can’t join all the sessions live? No problem. Your registration guarantees you access to the recorded lectures for a full year.
This bundle is specifically designed for healthcare professionals who want to learn more about diabetes fundamentals for their clinical practice or for those who are studying for the Certified Diabetes Care and Education Specialist (CDCES) exam.
Intended Audience: This library of critical information is designed for individuals or groups of diabetes specialists, including RNs, RDs, Pharmacists, Nurse Practitioners, Clinical Nurse Specialists, Physician Assistants, and other health care providers interested in staying up to date on current practices of care for people with diabetes and preparing for the CDCES Certification Exam.
All hours earned count toward your CDCES Accreditation Information
Sign up for Diabetes Blog Bytes – we post one daily Blog Byte from Monday to Friday. And of course, Tuesday is our Question of the Week. It’s Informative and FREE! Sign up below!
The use of DES products does not guarantee the successful passage of the CDCES exam. CBDCE does not endorse any preparatory or review materials for the CDCES exam, except for those published by CBDCE.