Question of Week | 1923 Noble Recipients for Discovery of Insulin?

To celebrate National Diabetes Month, our Questions of the Week will challenge test takers on their historical knowledge of the discovery of insulin. Thanks for joining us on this fun adventure.
In 1923, the Nobel Prize for in Medicine was awarded for the discovery of insulin.
Which group of scientists were the recipients for the award?
- Dr. Banting and Dr. Best
- Dr. Collip, Dr. Banting and Dr. Best
- Dr. Banting, Dr. Collip, Dr. Macleod, Dr. Best
- Dr. Banting and Dr. Macleod
Click Here to Test your Knowledge
Sign up for Diabetes Blog Bytes – we post one daily Blog Byte from Monday to Friday. And of course, Tuesday is our Question of the Week. It’s Informative and FREE! Sign up below!
[yikes-mailchimp form=”1″]The use of DES products does not guarantee the successful passage of the CDCES exam. CBDCE does not endorse any preparatory or review materials for the CDCES exam, except for those published by CBDCE.
Rationale of the Week | Cost of the Insulin Patent?

This month, we are quizzing test takers on the history of diabetes. Our November 16th Question of the week quizzed test takers on the cost of the insulin patent. 74% of respondents, chose the best answer. We are excited to share this info with you in celebration of National Diabetes Month.
Before we start though, if you don’t want any spoilers and haven’t tried the question yet, you can answer below: Answer Question
Question:
On January 23rd, 1923, Dr.’s Banting, Best, and Collip were awarded the patent for insulin.
How much did Banting, Best, and Collip each charge the University of Toronto for their share of the insulin patent?
Answer Choices:
- They sold the patent for insulin for one million dollars to be divided by the 3 patent owners.
- They retained the patent for insulin to ensure exclusive rights.
- They sold the patent for insulin for $1 each.
- They sold the patent for insulin to pharmaceutical companies for an undisclosed amount.
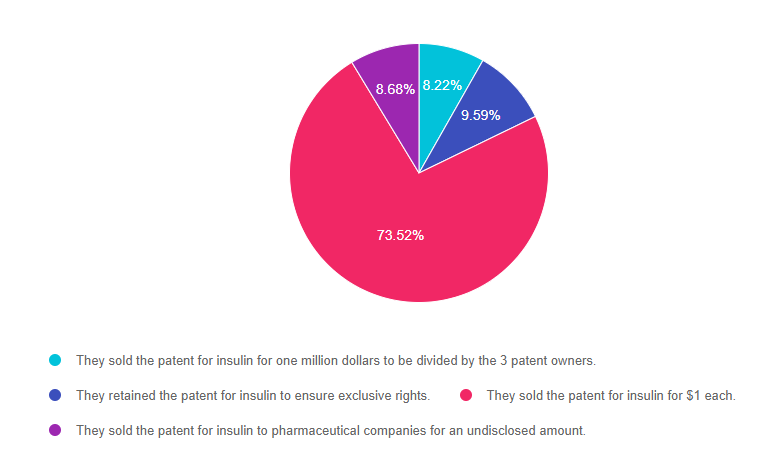
As shown above, the most common choice was option 3, the second most common answer was option 2, then option 4, and finally option 1.
Price of the Insulin Patent
On January 23rd, 1923 Banting, Best, and Collip were awarded the American patents for insulin. They sold the patent to the University of Toronto for $1 each. Banting notably said: “Insulin does not belong to me, it belongs to the world.” His desire was for everyone who needed access to it to have it.
In order for the insulin to be mass-produced and widely available, the pharmaceutical company Eli Lilly and Co. were given the right to do so. Currently, Eli Lilly, Sanofi, and Novo Nordisk are the major insulin producers. Insulin is no longer extracted from beef and pork pancreases. Now companies use E. coli and yeast to produce insulin through recombinant DNA therapy.
With insulin patents expiring, we are now seeing the approval of biosimilar insulins that come with lower price tags. This lower-cost insulin keeps Dr. Banting’s dream alive, which is to make insulin a gift that belongs to the world.
Answer 1 is incorrect. 8.22% chose this answer, “They sold the patent for insulin for one million dollars to be divided by the 3 patent owners.”
Answer 2 is incorrect. 9.59% of you chose this answer, “They retained the patent for insulin to ensure exclusive rights.”
Answer 3 is correct. 73.52% of respondents chose this answer, “They sold the patent for insulin for $1 each.” YES, GREAT JOB. This is the BEST ANSWER!
Finally, Answer 4 is incorrect. 8.68% chose this answer, “They sold the patent for insulin to pharmaceutical companies for an undisclosed amount.”
We hope you appreciate this week’s rationale! Thank you so much for taking the time to answer our Question of the Week and participate in this fun learning activity!
Want more practice questions? Enroll in our
Test Taking Practice Exam Toolkit Webinar
20 Sample Practice Questions
Join us live June 30, 2022, for live webinar 2022 updates
You are invited to join Coach Beverly for this FREE Webinar. And, if you want to have access to an additional 220+ sample practice online questions, you can purchase the complete Test Taking Toolkit.
For many of us, taking the certification exam is a nerve-wracking process.
During this webinar, Coach Beverly will help you transform your nervousness into focused energy that will help you succeed. She will provide test-taking tips based on her experience taking the certification exam six times.
2 Ways to Join Test Taking Webinar
Watch Webinar for FREE
This includes a review of 20 sample test questions with test-taking strategies. This does not include access to the recorded webinar or the practice questions.
Purchase for $49
This includes access to the recorded version of this webinar on your Online University Student Portal.
Plus, the Test Taking Toolkit provides you with over 220 sample online practice questions, simulating the exam experience. A perfect way to assess your knowledge and create a focused study plan, while increasing your test-taking confidence.
Don’t worry if you can’t make it live.
Your registration guarantees access to the recorded version.
Sign up for Diabetes Blog Bytes – we post one daily Blog Byte from Monday to Friday. And of course, Tuesday is our Question of the Week. It’s Informative and FREE! Sign up below!
[yikes-mailchimp form=”1″]Accreditation: Diabetes Education Services is an approved provider by the California Board of Registered Nursing, Provider 12640, and Commission on Dietetic Registration (CDR), Provider DI002. Since these programs are approved by the CDR it satisfies the CE requirements for the CDCES regardless of your profession.*
The use of DES products does not guarantee the successful passage of the CDCES exam. CBDCE does not endorse any preparatory or review materials for the CDCES exam, except for those published by CBDCE.
Rationale of the Week | What does “Diabetes Mellitus” really mean?

This month, we are quizzing test takers on the history of diabetes. Our November 9th Question of the week quizzed test takers on Diabetes Mellitus. 49% of respondents, chose the best answer. We are excited to share this info with you in celebration of National Diabetes Month.
Before we start though, if you don’t want any spoilers and haven’t tried the question yet, you can answer below: Answer Question
Question:
The term diabetes mellitus is derived from Greek and Latin languages, with roots dating back to the Greek physician Demetrius of Apamea in 129-199 AD.
Which is the most accurate translation of the term diabetes mellitus in English?
Answer Choices:
- Passing through of honey or sweetness.
- Siphoning of sugared urine.
- Wasting disease due to sweetness.
- Evil urinating disease.
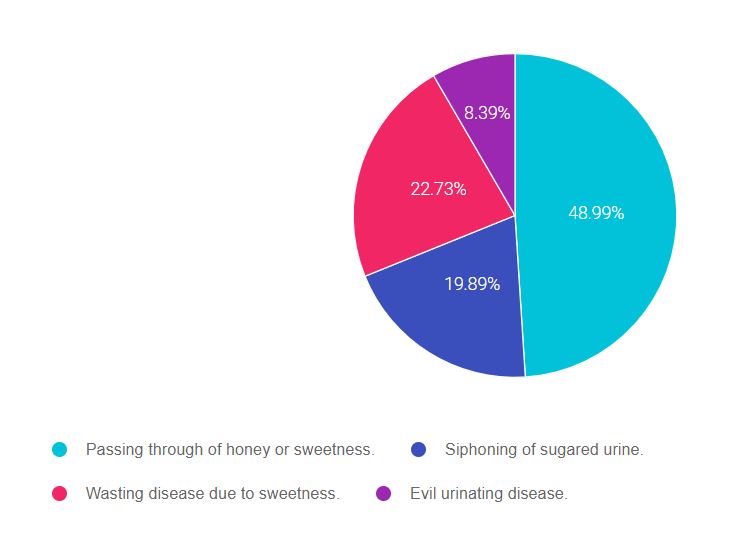
As shown above, the most common choice was option 1, the second most common answer was option 3, then option 2, and finally option 4.
Getting to the Best Answer
If you are thinking about taking the certification exam, this practice test question will set you up for success. Test writers anticipate possible answers based on the details in the question. They will wave those “juicy answers” that seem so familiar to you, right under your nose. Your job is to weed through, eliminate FALSE answers and then choose the BEST answer.
A short history of the evolution of the term “Diabetes mellitus“
The ancient Egyptians described clinical features of diabetes over 3000 years ago. Indian physicians called it madhumeha (‘honey urine’) because it attracted ants.
However, the term “diabetes” (Greek for ‘siphon’) was first used by Greek physician Demetrius of Apamea in 129-199 AD. The findings of sweet urine and blood was first noticed by ancient Indians. A few thousand years later, the Latin word “mellitus” (‘sweet like honey’) was coined by the British Surgeon-General, John Rollo in 1798.
History of the Islets and Insulin:
Paul Langerhans, 22 and working on his medical doctorate in 1869, identified the beta cells that came to be known as the ‘islets of Langerhans’. The name insulin was based on the secretions of the islets (Latin, insula = island). The term insulin was coined in 1909 and 1910, individually by de Mayer and Schaefer, respectively. Read more in this article, The History of Diabetes Mellitus, 2013 by Ritu Lakhtakia.
Answer 1 is correct. 48.99% chose this answer, “Passing through of honey or sweetness.” YES, GREAT JOB! The term “diabetes” is Greek for ‘siphon or passing through and the “mellitus” is Latin for “sweet like honey”.
Answer 2 is incorrect. 19.89% of you chose this answer, “Siphoning of sugared urine.” This is a juicy answer, but there is no Latin or Greek word for “urine” in the term “diabetes mellitus”.
Answer 3 is incorrect. 22.73% of respondents chose this answer, “Wasting disease due to sweetness.” Another juicy answer, but there is no Latin or Greek word for “wasting disease” in the term diabetes mellitus.
Finally, Answer 4 is incorrect. 8.39% chose this answer, “Evil urinating disease.” Some people might favor this term, but the term “diabetes mellitus” only describes the passing through of honey as a medical observation. There is no judgment associated with it.
Want to learn more about this fascinating topic? Read more in this article, The History of Diabetes Mellitus, 2013 by Ritu Lakhtakia.
We hope you appreciate this week’s rationale! Thank you so much for taking the time to answer our Question of the Week and participate in this fun learning activity!
Want more practice questions? Enroll in our
Test Taking Practice Exam Toolkit Webinar
20 Sample Practice Questions
Join us live December 16, 2021, for live webinar 2022 updates

You are invited to join Coach Beverly for this FREE Webinar. And, if you want to have access to an additional 220+ sample practice online questions, you can purchase the complete Test Taking Toolkit.
For many of us, taking the certification exam is a nerve-wracking process.
During this webinar, Coach Beverly will help you transform your nervousness into focused energy that will help you succeed. She will provide test-taking tips based on her experience taking the certification exam six times.
2 Ways to Join Test Taking Webinar
Watch Webinar for FREE
This includes a review of 20 sample test questions with test-taking strategies. This does not include access to the recorded webinar or the practice questions.
Purchase for $49
This includes access to the recorded version of this webinar on your Online University Student Portal.
Plus, the Test Taking Toolkit provides you with over 220 sample online practice questions, simulating the exam experience. A perfect way to assess your knowledge and create a focused study plan, while increasing your test-taking confidence.
Don’t worry if you can’t make it live.
Your registration guarantees access to the recorded version.
Sign up for Diabetes Blog Bytes – we post one daily Blog Byte from Monday to Friday. And of course, Tuesday is our Question of the Week. It’s Informative and FREE! Sign up below!
[yikes-mailchimp form=”1″]Accreditation: Diabetes Education Services is an approved provider by the California Board of Registered Nursing, Provider 12640, and Commission on Dietetic Registration (CDR), Provider DI002. Since these programs are approved by the CDR it satisfies the CE requirements for the CDCES regardless of your profession.*
The use of DES products does not guarantee the successful passage of the CDCES exam. CBDCE does not endorse any preparatory or review materials for the CDCES exam, except for those published by CBDCE.
New Treatment for Type 1 Diabetes | VX-880
Vertex Pharmaceuticals just announced preliminary results from a trial that explores a new intervention to treat type 1 diabetes. The early results are very promising.
The first person with type 1 diabetes to receive this new stem-cell derived experimental therapy, had an 91% drop in their insulin needs. The person has lived with type 1 for over 40 years. After the intervention, they not only experienced a reduction in their insulin needs, their fasting C-peptide levels went from undetectable to 280. This dramatic C-peptide increase is a clinical indicator of stem-cell therapy success and endogenous insulin secretion.
These results are exciting and offer hope for a potential new treatment approach for type 1 diabetes.
VX-880 is a stem cell derived therapy that replaces damaged beta cells with healthy transplanted insulin producing cells in clinical trials. However, these new cells are at risk for attack by the body’s immune system, so immunosuppression therapy is currently required for stem-cell transplant success.
The future goal is to create a version of this treatment that doesn’t require immunosuppressive therapy. And Vertex, the makers of VX-880 are working on creating an encapsulated islet cell program that doesn’t initiate an autoimmune attack.
For more information and clinical trials, click this link.
Resources for People Living with Type 1 Diabetes

Below is a list of helpful online resources for Type 1 Diabetes. They include sites for national organizations like the American Diabetes Association (ADA), sites for diabetes interest groups, and other participant organizations that provide helpful diabetes tips and opportunities to join online groups. Click here for a Type 1 Resource Handout to share with colleagues and people living with type 1 diabetes.
Click the links below to visit the website:
- Let’s fight Type 1 Together | American Diabetes Association (ADA)
- Mental Health Resources Directory | ADA
- Type 1 Diabetes Resources and Support | Juvenile Diabetes Research Foundation: Explore our informational guides or make a personal connection with someone experienced with type 1 diabetes (T1D). The JDRF community has you covered.
- Empowering Youth with Type 1 Diabetes |The Chris Dudley Foundation
- The National Institutes of Health Diabetes Resources | CDC
- The College Diabetes Network: Focuses Specifically on Young Adults with Diabetes | College Diabetes Network
- The Diabulimia Helpline: for Individuals Having Eating Problems
- Beyond Type 1 Diabetes
- Connected in Motion: Peer-Based Sports & Outdoor Adventures for those with Type 1 (in U.S. and Canada) | Connected In Motion
- Diatribe: Library of Online Resources, Blog & Community Forums
- Diabetes Education: At times it might seem overwhelming, but you can thrive with diabetes, and a Diabetes Care and Education Specialist can help. Includes a link to find a diabetes program near you.
Sign up for Diabetes Blog Bytes – we post one daily Blog Byte from Monday to Friday. And of course, Tuesday is our Question of the Week. It’s Informative and FREE! Sign up below!
[yikes-mailchimp form=”1″]Question of Week | Cost of the Insulin Patent?

To celebrate National Diabetes Month, our Questions of the Week will challenge test takers on their historical knowledge of the discovery of insulin. Thanks for joining us on this fun adventure.
On January 23rd, 1923, Dr.’s Banting, Best, and Collip were awarded the patent for insulin.
How much did Banting, Best, and Collip each charge the University of Toronto for their share of the insulin patent?
- They sold the patent for insulin for one million dollars to be divided by the 3 patent owners.
- They retained the patent for insulin to ensure exclusive rights.
- They sold the patent for insulin for $1 each.
- They sold the patent for insulin to pharmaceutical companies for an undisclosed amount.
Click Here to Test your Knowledge
Join us in January for our
Level 1 | Diabetes Fundamentals 2022 Live Updates
9+ CEs | $109
2022 Updates Airs January 11th-27th, 2022
This bundle is specifically designed for healthcare professionals who want to learn more about diabetes fundamentals for their clinical practice or for those who are studying for the Certified Diabetes Care and Education Specialist (CDCES) exam.
2022 Live Webinar Updates
- January 11, 2022 – Class 1 – Getting to the Nitty Gritty 1.5 CEs
- January 13, 2022 – Class 2 -Nutrition and Exercise 1.5 CEs
- January 18, 2022 – Class 3 – Insulin Therapy & Pattern Management 1.5 CEs
- January 20, 2022 – Class 4 – Meds Overview for Type 2 – 1.5 CEs
- January 25, 2022 – Class 5 – Goals of Care – 1.5 CEs
- January 27, 2022 – Class 6 – Hypoglycemia, Sick Days, Monitoring, Foot Care 1.5 CEs
Sign up for Diabetes Blog Bytes – we post one daily Blog Byte from Monday to Friday. And of course, Tuesday is our Question of the Week. It’s Informative and FREE! Sign up below!
[yikes-mailchimp form=”1″]Accreditation: Diabetes Education Services is an approved provider by the California Board of Registered Nursing, Provider 12640, and Commission on Dietetic Registration (CDR), Provider DI002. Since these programs are approved by the CDR it satisfies the CE requirements for the CDCES regardless of your profession.*
The use of DES products does not guarantee the successful passage of the CDCES exam. CBDCE does not endorse any preparatory or review materials for the CDCES exam, except for those published by CBDCE.
Faculty of Virtual DiabetesEd Specialist Conference – 2022
Faculty of Virtual DiabetesEd Specialist Conference
Coach Beverly Thomassian, RN, MPH, BC-ADM, CDCES

Author, Nurse, Educator, Clinician and Innovator, Beverly has specialized in diabetes management for over twenty years. As president and founder of Diabetes Educational Services, Beverly is dedicated to optimizing diabetes care and improving the lives of those with diabetes.
Diana Isaacs, PharmD, BCPS, BC-ADM, BCACP, CDCES

We are thrilled to welcome our newest speaker, Diana Isaacs, who will be joining our Virtual and Live Courses!
Dr. Isaacs was named 2020 AADE Diabetes Educator of the Year for her educational platform promoting the use of CGM for people with diabetes and other innovations. Dr. Isaacs was awarded the Ohio Pharmacists Association Under 40 Award in 2019. Dr. Isaacs has served in leadership roles for several pharmacies and diabetes organizations. She has numerous diabetes publications and research projects with a focus on medications, CGM and diabetes technology.
As the CGM Program Coordinator and clinical pharmacist specialist in the Cleveland Clinic Diabetes Center, Dr. Isaacs brings a wealth of clinical knowledge combined with extensive research experience to this program.
Read interview with Dr. Isaacs here!
Ashley LaBrier, MS, RD, CDCES

Ashley is an educator, dietitian, and Diabetes Education Program Coordinator at the Salinas Valley Medical Clinic’s Diabetes & Endocrine Center. Her work with people living with diabetes focuses on the value of healthy nutrition and movement to improve well-being.
Ashley is passionate about providing person-centered education to empower those who live with diabetes. Having been diagnosed with type 1 diabetes herself nearly 20 years ago, she combines her professional knowledge with personal experience and understanding.
Read interview with Ms. LaBrier here!
Virtual DiabetesEd Specialist Conference Schedule Coming Soon!
April 13 with Coach Beverly and Dr. Diana Isaacs
8:00—12:00 pm | BREAK | 1:00— 4:30 pm PST
Topics Include:
- Current State of Diabetes ADA Standards of Care
- Person Centered Care for Type 1, Type 2, LADA, GDM
- Medical Evaluation, Risk Identification
- Diabetes Prevention
- Glycemic targets across the Lifespan
- Hypoglycemia prevention & treatment
- Landmark Studies
- Medications for Type 2
- Pharmacology Algorithms – AACE and ADA
- Cardiovascular Monitoring and Management
- Delivering Extraordinary Diabetes Care
April 14 with Coach Beverly and Dr. Diana Isaacs
8:00—12:00 pm | BREAK | 1:00— 4:30 pm PST
- Insulin – The Ultimate Hormone Replacement Therapy
- Insulin Pattern Management and Dosing Strategies
- Diabetes Interview – From Head to Toe
- Microvascular Risk Reduction
- Diabetes Technology—Monitors, Pumps & Data Interpretation
- Integrating Mental Health with Body Health
- Assessment Tools, Recognizing Trauma and Self-Care Strategies
April 15 with Ashley LaBrier, MS, RD, CDCES
8:00 am—Noon
- Medical Nutrition Therapy Overview
- Micro and Macronutrients
- Evidence based approaches to MNT
- Meal Planning – How to Eat by the Numbers
- Keeping Well Through Activity and Nutrition
*Dates and times subject to change
Accreditation: Diabetes Education Services is an approved provider by the California Board of Registered Nursing, Provider 12640, and Commission on Dietetic Registration (CDR), Provider DI002. Since these programs are approved by the CDR it satisfies the CE requirements for the CDCES regardless of your profession.*
The use of DES products does not guarantee the successful passage of the CDCES exam. CBDCE does not endorse any preparatory or review materials for the CDCES exam, except for those published by CBDCE.
Preparing for BC-ADM Exam? Learn about Exam updates at Free Webinar | Nov. 17th
Are you Preparing for the BC-ADM Exam?
We have some exciting exam updates to share.
Join Coach Beverly, Wednesday November 17th at 11:30 am PST for everything you need to know to prepare!

Becoming Board Certified in Advanced Diabetes Management (BC-ADM) provides an opportunity for diabetes specialists with an advanced degree in their field (plus a professional license as an advanced practice nurse, registered dietitian, registered pharmacist, or provider) to increase the breadth and depth of their diabetes knowledge. The scope of advanced diabetes practice includes management skills such as medication adjustment, medical nutrition therapy, exercise planning, counseling for behavior management, and psychosocial issues.
Attaining optimal diabetes management includes using a person-centered approach coupled with assessment, screening, management, and monitoring of acute and chronic diabetes co conditions. This webinar will review changes in requirements for 2021, exam eligibility and test format, strategies to succeed along with a review of study tips and test-taking tactics. We will review sample test questions and the reasoning behind choosing the right answers. We hope you can join us for this webinar.
Can’t join us live? No worries! Registrants get priority notification and link to recorded version within 24 hours.
Save the Date for our Cyber Monday Sale!

For one day only, save 25% off all of our Online Courses!
Use code “CYBER25” on the payment page during checkout on November 30th
WANT A REMINDER EMAIL BEFORE THE SALE?
Sign up for Diabetes Blog Bytes – we post one daily Blog Byte from Monday to Friday. And of course, Tuesday is our Question of the Week. It’s Informative and FREE! Sign up below!
[yikes-mailchimp form=”1″]
Accreditation: Diabetes Education Services is an approved provider by the California Board of Registered Nursing, Provider 12640, and Commission on Dietetic Registration (CDR), Provider DI002. Since these programs are approved by the CDR it satisfies the CE requirements for the CDCES regardless of your profession.*
The use of DES products does not guarantee the successful passage of the CDCES exam. CBDCE does not endorse any preparatory or review materials for the CDCES exam, except for those published by CBDCE.
Rationale of the Week | The First Person to Receive Insulin?

This month, we are quizzing test takers on the history of diabetes and the discovery of insulin. Our November 2nd Question of the week quizzed test takers on the first insulin injections in humans. 47% of respondents, chose the best answer. We are excited to share this info with you in celebration of National Diabetes Month.
Before we start though, if you don’t want any spoilers and haven’t tried the question yet, you can answer below: Answer Question
Question:
Which of the following statements is true regarding the first experiments using insulin in humans?
Answer Choices:
- Since insulin worked successfully on dogs, no experimentation was needed on humans to gain approval.
- Leonard Thompson, a 14-year-old received the first successful insulin injection in January 1922.
- The initial insulin was derived from the exocrine cells of ligated canine and porcine pancreases.
- Elizabeth Hughes was the first insulin recipient in 1921 but the insulin formulation didn’t work to lower her glucose until 1922.
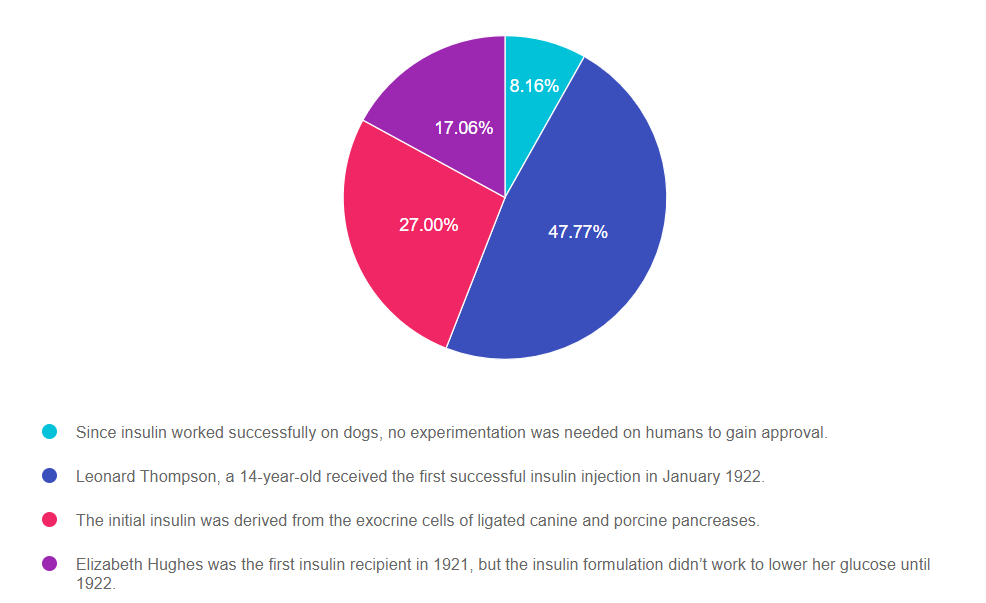
As shown above, the most common choice was option 2, the second most common answer was option 3, then option 4, and finally option 1.
Getting to the Best Answer
If you are thinking about taking the certification exam, this practice test question will set you up for success. Test writers anticipate possible answers based on the details in the question. They will wave those “juicy answers” that seem so familiar to you, right under your nose. Your job is to weed through, eliminate FALSE answers and then choose the BEST answer.
Answer 1 is incorrect. 8.16% chose this answer, “Since insulin worked successfully on dogs, no experimentation was needed on humans to gain approval.” Insulin’s approval was certainly fast tracked, but experiments were conducted on animals first, than humans, before releasing for widespread use and saving the lives of millions.
Answer 2 is correct. 47.77% of you chose this answer, “Leonard Thompson, a 14-year-old received the first successful insulin injection in January 1922.” YES, great job. On January 11, 1922, Leonard Thompson was the first person to receive insulin when he was only 14 years of age. The first injection caused an allergic reaction due to impurities. After James Collip improved the insulin refinement process, the second dose of canine pancreas extract was delivered to the young patient twelve days after the first. Thompson’s health rapidly improved and he lived another 13 years on insulin injections, dying at the young age of 26 due to pneumonia.
Answer 3 is incorrect. 27% of respondents chose this answer, “The initial insulin was derived from the exocrine cells of ligated canine and porcine pancreases.” This is a juicy sounding answer! However, insulin was derived from the endocrine cells of dogs, ox and porcine, to produce insulin; not the exocrine cells that produce digestive enzymes.
Finally, Answer 4 is incorrect. 17.06% chose this answer, “Elizabeth Hughes was the first insulin recipient in 1921 but the insulin formulation didn’t work to lower her glucose until 1922.” Another juicy answer since it has some elements of truth, however Elizabeth was not the first person to receive insulin therapy. Elizabeth developed diabetes in 1918 at age 11 and by the fall of 1922, she weighed only 45 pounds, due to her body’s inability to store energy and the strict 800 calorie diet she followed to prevent ketosis. Elizabeth arrived in Toronto in August 15, 1922 and received insulin injections from Dr. Banting and she recovered rapidly. She returned home to Washington D.C . Thanksgiving Day 1922 on a 2200 calorie meal plan and insulin injections. She lived to the age of 73, and received over 42,000 insulin injections over her lifetime. You can read more in the book, Breakthrough, which chronicles Elizabeth Hughes, the discovery of insulin and the Making of a Medical Miracle.
More Reading on the Discovery of Insulin
The Discovery of Insulin – Vecchio I, Tornali C, Bragazzi NL, Martini M. The Discovery of Insulin: An Important Milestone in the History of Medicine. Front Endocrinol (Lausanne). 2018;9:613. Published 2018 Oct 23. doi:10.3389/fendo.2018.00613
Breakthrough, which chronicles Elizabeth Hughes, the discovery of insulin and the Making of a Medical Miracle.
We hope you appreciate this week’s rationale! Thank you so much for taking the time to answer our Question of the Week and participate in this fun learning activity!
Enroll in our Virtual DiabetesEd Specialist Program!
Did you miss the live conference? No worries!
You can register now to watch on-demand
Click here to learn more and get started!
Whether you are new to diabetes or a seasoned expert, you’ll benefit from this virtual conference with the latest research plus critical content that you can immediately apply to your clinical practice.
If you are seeking a state-of-the-art review of current diabetes care, this course is for you. Our team has been fine-tuning this course for over fifteen years, and we know what you need. This program can also be a great addition to your CDCES or BC-ADM exam study plan.
Team of expert faculty includes:
- Diana Isaacs, PharmD, BCPS, BC-ADM, BCACP, CDCES – Educator of the Year, 2020
- Coach Beverly Thomassian, RN, MPH, CDCES, BC-ADM
- Ashley LaBrier, MS, RD, CDCES, Diabetes Program Coordinator
In addition to informative lectures, we also use group activities and case studies to highlight the essential knowledge, skills, and strategies needed to succeed in diabetes education today!
CEs: Includes over 30 CEs
Program Info: 2021 Diabetes Educator Course Flyer & Schedule (subject to change)
Speakers: View Conference Faculty.
Dates: Your registration fee includes access to FREE podcast and all recorded webinars for one year.
Virtual DiabetesEd Specialist Conference Deluxe | Recorded & Ready for Viewing! | 30+ CEs
Deluxe Virtual Program for $459 includes:
- Presentations by our team of experts
- Q & A Session with the instructor after each webinar
- State-of-the-art review of current diabetes care and technology.
- Resources for each session
- Access to FREE podcast and recorded webinars within a week of each live session for one full year.
+Plus Syllabus, Standards and Swag:
- Diabetes Educator Course 2021 Syllabus Hard Copy – over 100 pages -This spiral-bound workbook contains the printed version of all of the instructor’s slides.
- DiabetesEd Services highlighters, Medication PocketCard and Pen
2021 Diabetes Educator Course Flyer & Schedule (subject to change)
Team of Experts: Our team of expert faculty has been fine-tuning this course for over fifteen years and we know what you need to succeed! In addition to informative lectures, we also use group activities and case studies to highlight the essential knowledge, skills, and strategies needed to succeed in diabetes education today!
Bonus Courses worth 12+ CEs, FREE
When you register for our Virtual Course, you have immediate access to these Bonus DiabetesEd University Online Courses – for FREE!
- Test Taking Toolkit – Over 200 sample test questions!
- Level 2 – Assessing and Promoting Well-Being: From Population Health to a Person-Centered Approach 1.5 CEs
- Level 2 – Hospital and Hyperglycemia 1.5 CEs
- Level 2 – Hyperglycemic Crisis, DKA and HHS Standards 1.0 CEs
- Level 2 – Meds Management Update for Type 2 – 1.5 CEs
- Level 2 – Setting up a Successful Diabetes Program 1.5 CEs
- Level 2 – Pregnancy and Diabetes 1.5 CEs
- Level 2 – From Tots to Teens – Diabetes Standards 1.5 CEs
- Level 2 – Older Adults and Diabetes 1.5 CEs
- Mindfulness and Compassion in the Diabetes Encounter – 1.0 CE
2021 Diabetes Educator Course Flyer & Schedule (subject to change)
Sign up for Diabetes Blog Bytes – we post one daily Blog Byte from Monday to Friday. And of course, Tuesday is our Question of the Week. It’s Informative and FREE! Sign up below!
[yikes-mailchimp form=”1″]Accreditation: Diabetes Education Services is an approved provider by the California Board of Registered Nursing, Provider 12640, and Commission on Dietetic Registration (CDR), Provider DI002. Since these programs are approved by the CDR it satisfies the CE requirements for the CDCES regardless of your profession.*
The use of DES products does not guarantee the successful passage of the CDCES exam. CBDCE does not endorse any preparatory or review materials for the CDCES exam, except for those published by CBDCE.








