What Changed with the New DSMES Standard? Nine Takeaways
If you want to get fired up about providing Diabetes Self Management and Education Support (DSMES), the newly updated Standards for DSMES is highly recommended reading. If you don’t have time to read the complete document, we have provided our top 9 takeaways to get you started.
Every 5 years, a committee of diabetes education specialists and advocates gets together to update this roadmap for the provision of DSMES. In the last version of this document, there were ten standards and lots of complicated rules and regulations required to set up a recognized DSMES Program.
In this new version, the collaborative of authors possesses a fresh outlook and clear vision that resulted in six simplified standards with the goal of inclusivity and breaking down barriers.
To address inequities, a candid discussion of racial disparities and social determinants of health is included. In addition, there is recognition that participation in DSMES has lost momentum during the pandemic with stagnant or decreasing enrollment. We need to innovate and make access and participation a top priority to make sure all people have the opportunity to benefit from this knowledge and life-saving information.
Coach Beverly’s 9 Takeaways from updated DSMES Standard.
- I love the definition they included of a CDCES – “A compassionate teacher and expert who, as an integral member of the care team, provides collaborative, comprehensive, and person-centered care and education for people with diabetes”. This is the best description of our caring expertise and role in improving care.
2. DSMES makes a difference! – Lowers A1c by at least 0.6% with greater A1c reductions when engaging in DSMES of 10 hours or more. In addition, DSMES has a positive effect on clinical, psychosocial, and behavioral aspects while improving quality of life and coping skills. Individuals who participate are more likely to engage in self-care through behavior change, including eating healthier eating and regular exercise.
3. Breaking down barriers through recognition of Social Determinants of Health and addressing equity. The authors recognize the need for person-centered services that embrace cultural differences, social determinants of health, and ever-increasing technological engagement platforms and systems. The goal is to increase health equity through access to this critical service while focusing more on person-centered care and decreasing administrative complexities.
4. Recognition of the need for a thoughtful community needs assessment that looks at more than demographics. We still need to gain data from local and national resources to identify race, ethnicity, cultural background, sex, age, geographic location, tech access, and literacy. But just as important are the perceptions of risk associated with diabetes and barriers including socioeconomics, cultural factors, misaligned schedules, and health insurance shortfalls.
5. An important and often underappreciated barrier to DSMES includes perceived lack of need and limited encouragement from health care professionals to engage in DSMES. Plus, special attention needs to be payed to those who do not usually attend clinic appointments to discover their perceived and real barriers.
6. Diabetes Care Community Coordinators are needed to help build bridges between the medical community and the community we serve. These individuals include community health workers and health promoters who live in the community and have familiarity and understanding of the needs and cultural factors of the individuals we are seeking to serve. Diabetes care coordinators also include; dietetic technicians, medical assistants, peer educators, and leaders. They can instruct, reinforce self-management skills, support behavior change, facilitate group discussion and provide social support.
7. Keep the curriculum dynamic and practical. Research endorses the inclusion of practical, problem-solving approaches, collaborative care, consideration of psychosocial issues, and support of behavior change strategies to sustain self-management efforts. In addition, supplementing with resources and support materials can help individuals navigate the health care system and promote self-advocacy.
8. Strategies to increase DSMES participation through provider referrals. Keeping programs vibrant and active is no easy task and requires constant attention. I put together a list of strategies I have used to boost referrals by providers. Direct mail of DSMES flyers to providers, networking during community gatherings, lunch and learn CE activities, hallway conversations, welcome packet for new providers, delivery of referral forms and holiday gifts to offices, and shared participant testimonials.
9. Strategies to increase DSMES participation through self-referrals. We can directly appeal to our community members and then reach out to their providers to approve the referral f. Ideas to touch your community include; publishing articles on hot diabetes topics, sending out press releases, advertising in local papers and on social media, hosting events during National Diabetes Month, joining health fairs, providing community presentations to service organizations, and promoting word of mouth marketing with your graduates.
Diabetes Self-Management Education and Support is a critical components of comprehensive diabetes care. By addressing barriers and including community members in our outreach, we can break down the walls and increase participation and improve the quality of life for all people.
Want to learn more about this topic? Enroll in our
Setting up a Successful DSME Program Standards Webinar | Level 2 $29 | 1.5 CEs
Recorded & Ready to Watch!
This course provides you with a succinct overview of the latest standards for Diabetes Self-Management Education (DSME) and Support Programs. If you are taking certification exams or considering setting up a DSME program, this program is designed for you. We highlight the newly revised and simplified 2022 Standards and provide strategies on program implementation. In addition, we discuss Medicare Reimbursement and covered benefits. This course provides insights into the exam philosophy and also highlights critical content areas.
Objectives:
- Describe DSME program examples from across the country.
- List the six standards for creating a successful DSME program
- Discuss marketing strategies for success
- Describe Medicare Reimbursement for diabetes care and education
Join us for our Virtual DiabetesEd Specialist Conference
30+ CEs | April 13-15, 2022
Whether you are new to diabetes or a seasoned expert, you’ll benefit from this virtual conference with the latest research plus critical content that you can immediately apply to your clinical practice.
If you are seeking a state-of-the-art review of current diabetes care, this course is for you. Our team has been fine-tuning this course for over fifteen years, and we know what you need. This program can also be a great addition to your CDCES or BC-ADM exam study plan.
Download Course Schedule | Download Course Flyer
Join us LIVE for this Virtual Course and enjoy a sense of community!
Team of expert faculty includes:
- Diana Isaacs, PharmD, BCPS, BC-ADM, BCACP, CDCES – Educator of the Year, 2020
- Coach Beverly Thomassian, RN, MPH, CDCES, BC-ADM
- Ashley LaBrier, MS, RD, CDCES, Diabetes Program Coordinator
Download Course Schedule | Download Course Flyer
Two Registration Options
Virtual DiabetesEd Specialist Conference Deluxe | 30+ CEs
Deluxe Option for $499: Virtual Program includes:
- Q & A Session with the instructor after each webinar.
- LIVE Presentations by our team of experts.
- State of the art review of current diabetes care and technology.
- Resources for each session.
- Access to free podcasts and video recordings within a week of each live session for one year.
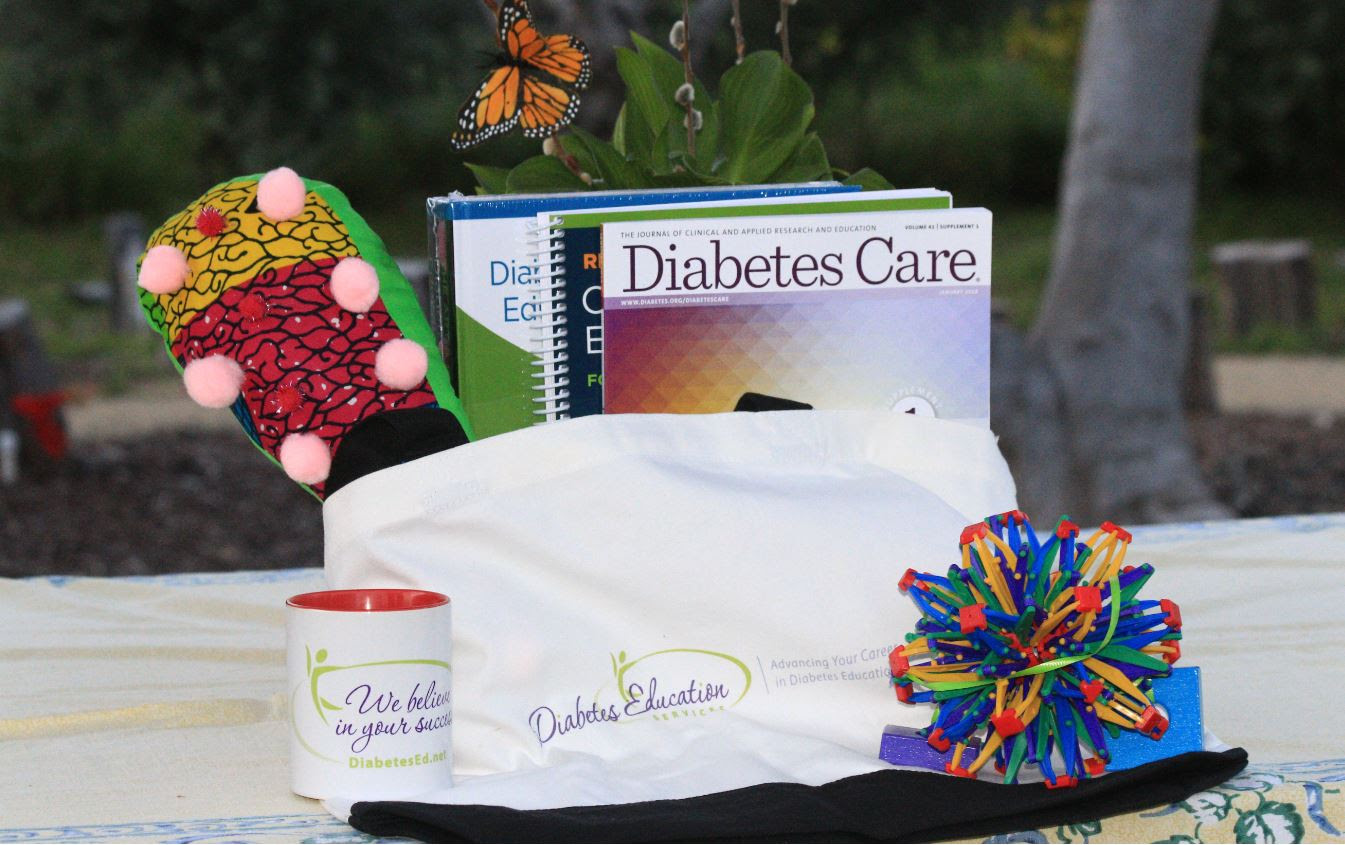
Deluxe Version includes Syllabus, Standards and Swag*:
- Diabetes Educator Course 2022 Syllabus Hard Copy – over 100 pages -This spiral-bound workbook contains the printed version of all of the instructor’s slides.
- ADA 2022 Standards of Care Book -The ADA Standards of Medical Care in Diabetes is a key resource for healthcare professionals involved in diabetes care, education, and support.
- DiabetesEd Services highlighters, Medication PocketCard, Tote Bag and Pen
Virtual DiabetesEd Specialist Conference Basic | 30+ CEs
Deluxe Option for $499: Virtual Program includes:
- Q & A Session with the instructor after each webinar.
- LIVE Presentations by our team of experts.
- State of the art review of current diabetes care and technology.
- Resources for each session.
- Access to free podcasts and video recordings within a week of each live session for one year.
Don’t worry if you can’t make it live. Your registration guarantees access to the recorded version in the Online University.
All hours earned count toward your CDCES Accreditation Information
Sign up for Diabetes Blog Bytes – we post one daily Blog Byte from Monday to Friday. And of course, Tuesday is our Question of the Week. It’s Informative and FREE! Sign up below!
The use of DES products does not guarantee the successful passage of the CDCES exam. CBDCE does not endorse any preparatory or review materials for the CDCES exam, except for those published by CBDCE.
Reducing 4 Risk Factors in Diabetes can Add Years to One’s Life
Having diabetes is a lot of work. We ask participants with diabetes to change their eating habits, drink water, move more, take a bunch of medications and attend diabetes classes plus see providers on a regular basis. In addition, we collaborate with and encourage them to get their ABC’s (A1C, Blood pressure, Cholesterol) to target.
Is worth all the work?

The short answer is YES. Making these hard fought behavior changes can add years to one’s life.
A recent study published in the JAMA Network last month suggests that people living with Type 2 Diabetes can increase life expectancy by reducing 4 risk factors and hitting specific metabolic targets.
This study evaluated life expectancy increases among 421 people living with type 2 diabetes for those who reduced A1C, systolic blood pressure (SBP), low-density lipoprotein cholesterol (LDL-C), and body mass index (BMI) with each biometer goal was broken into quartiles.
A message of hope
Providers can shine a light on these findings to encourage people with diabetes to make those difficult behavior changes, and to keep working at it when the going gets tough. Their efforts do make a difference in improving life expectancy and daily quality of life.
Reducing A1C
Participants who reduced their A1C saw the highest increase in life expectancy compared to the other biometers. For those with the highest A1Cs, lowering their levels added years to their life expectancy.
- Fourth Quartile – The individuals who were able to bring their A1C’s down to 5.9% that started in the highest quartile at an average of 9.9% saw an average of 3.8 years added to their life expectancy.
- Third Quartile – Those who brought it down to 7.7% from 9.9% in the third quartile saw an average 3.4-year gain.
- Second Quartile – Participants in the second quartile with a change of 7.7% to 6.8% only saw a 0.5-year change in life expectancy.
- First Quartile – No change in life expectancy was seen for those in this quartile who went from a 6.8% HbA1c down to 5.9% HbA1c.
Lowering Systolic Blood Pressure
Lowering blood pressure added just over a year to the participant’s life expectancy.
- Fourth Quartile: The average baseline blood pressure was 160.4 mm Hg
- Third Quartile: Participants with a 139.1 mm Hg saw 1.1 years gained in life expectancy.
- Second Quartile: A 128.2 mm Hg was associated with a 1.5-year gain in life expectancy.
- First Quartile: The highest increase in life expectancy for blood pressure was for those at 114.1 mm Hg with a 1.9 year gain.
Lowering LDL Cholesterol
Participants with lower LDL cholesterol, saw a change in life expectancy by a few months.
- Fourth Quartile: The baseline was 146.2 mg/dL.
- Third Quartile: Those who had a 107.0 mg/dL saw a half-year increase in life expectancy.
- Second Quartile: Those who had an 84.0 mg/dL saw a 0.7 year gain in life expectancy.
- First Quartile: Individuals who had a 59 mg/dL saw a 0.9-year gain in life expectancy.
Lowering Body Mass Index
Participants who were able to decrease their BMI saw a increased life expectancy by a few years.
- Fourth Quartile: The baseline BMI was 41.4 (fourth quartile) with the lower three quartiles seeing a change in life expectancy.
- Third Quartile: For individuals with a BMI of 33.0, they saw an additional 2 years of life expectancy
- Second Quartile: Those who had a BMI of 28.6 saw an additional 2.9 years of life expectancy
- First Quartile: Those living with Type 2 with a BMI of 24.3 see an additional 3.9 years of life expectancy
Smoking cessation also had an impact with 0.7 years added for women aged 50 to 60 years and 1.1 years for men aged 70 to 80 years of age.
Overall, we hope this news brings hope to those living with Type 2 diabetes and improves care knowing that reaching these goals can extend their lifetime.
To read more click here and here.
Join us live next Tuesday and Thursday as we continue our Level 2 – Standards of Care Intensive live updates! Read more and enroll below.
Sign up for Diabetes Blog Bytes – we post one daily Blog Byte from Monday to Friday. And of course, Tuesday is our Question of the Week. It’s Informative and FREE! Sign up below!
The use of DES products does not guarantee the successful passage of the CDCES exam. CBDCE does not endorse any preparatory or review materials for the CDCES exam, except for those published by CBDCE.
March eNews | Rediscovering the Magic of Nutrition

Happy March
Join us in celebration of National Nutrition Month!
We have a whole month to celebrate the healing properties of food and the daunting expertise and abundant knowledge of our nutrition colleagues.
Did you know that people with diabetes who meet with a RD/RDN have a 1-2% drop in A1c?
Dietitians are smart, evidence-based, caring advocates and some of my favorite people. Plus, they have the best teaching tools (who doesn’t love the measuring cups, food models and empty cereal boxes?).
For this newsletter, we focus on the impact of nutrition on health.
We reveal the best rated meal plan and highlight how it earned the number one ranking. We also tackle the topic of B12 deficiency for those on metformin therapy. Plus, we rekindle the magic and memory of fruits and vegetables with the hopes of increasing consumption. Lastly, we detail the recently approved implantable CGM, that only needs to be changed twice a year.
We hope you enjoy our nutrition inspired Question and Rationale of the Week. And, you are invited to attend our Virtual Conference, where we dedicate an entire four hours to MNT, with our expert speaker, Ashley LaBrier, MS, RD, CDCES.
Happy Nutrition Month everyone! In health,
Beverly, Bryanna, Jackson, and Amanda
Click here to read our full March 2022 newsletter.
Featured Articles
- Best rated meal plan
- Metformin and B12 deficiency
- Magic of fruit & veggies
- New implantable CGM
- Question of the Week
- Rationale of Week
Upcoming Webinars
Featured Items
- ADCES Book Bundle
- Swag
- Free Resources
Join our Virtual DiabetesEd Specialist Conference
30+ CEs | April 13-15, 2022

Whether you are new to diabetes or a seasoned expert, you’ll benefit from this virtual conference with the latest research plus critical content that you can immediately apply to your clinical practice.
If you are seeking a state-of-the-art review of current diabetes care, this course is for you. Our team has been fine-tuning this course for over fifteen years, and we know what you need. This program can also be a great addition to your CDCES or BC-ADM exam study plan.
Download Course Schedule | Download Course Flyer
Join us LIVE for this Virtual Course and enjoy a sense of community!
Team of expert faculty includes:
- Diana Isaacs, PharmD, BCPS, BC-ADM, BCACP, CDCES – Educator of the Year, 2020
- Coach Beverly Thomassian, RN, MPH, CDCES, BC-ADM
- Ashley LaBrier, MS, RD, CDCES, Diabetes Program Coordinator
Two Registration Options
Virtual DiabetesEd Specialist Conference Deluxe | 30+ CEs
Deluxe Option for $499: Virtual Program includes:
- Q & A Session with the instructor after each webinar.
- LIVE Presentations by our team of experts.
- State of the art review of current diabetes care and technology.
- Resources for each session.
- Access to free podcasts and video recordings within a week of each live session for one year.
Deluxe Version includes Syllabus, Standards and Swag*:
- Diabetes Educator Course 2022 Syllabus Hard Copy – over 100 pages -This spiral-bound workbook contains the printed version of all of the instructor’s slides.
- ADA 2022 Standards of Care Book -The ADA Standards of Medical Care in Diabetes is a key resource for healthcare professionals involved in diabetes care, education, and support.
- DiabetesEd Services highlighters, Medication PocketCard, Tote Bag and Pen
Virtual DiabetesEd Specialist Conference Basic | 30+ CEs
Deluxe Option for $499: Virtual Program includes:
- Q & A Session with the instructor after each webinar.
- LIVE Presentations by our team of experts.
- State of the art review of current diabetes care and technology.
- Resources for each session.
- Access to free podcasts and video recordings within a week of each live session for one year.
Don’t worry if you can’t make it live. Your registration guarantees access to the recorded version in the Online University.
All hours earned count toward your CDCES Accreditation Information
Sign up for Diabetes Blog Bytes – we post one daily Blog Byte from Monday to Friday. And of course, Tuesday is our Question of the Week. It’s Informative and FREE! Sign up below!
The use of DES products does not guarantee the successful passage of the CDCES exam. CBDCE does not endorse any preparatory or review materials for the CDCES exam, except for those published by CBDCE.
Earth Day Secrets to Improving Planet Health
January eNews | New 2022 Diabetes Standards – Screening Updates and Cheat Sheets
January eNews | New 2022 Diabetes Standards – Screening Updates and Cheat Sheets
Happy New Year
January kicks off our ADA Standards of Care (SOC) celebration and exploration. Coach Beverly has discovered some real gems that she is excited to share with all of you.
“By implementing and championing these evidence-based guidelines, we can make a significant impact in improving care.”
Our goal is to highlight key areas and changes to the standards that will benefit people with diabetes the most.
In this first newsletter of 2022, we feature the new screening guidelines for prediabetes and diabetes. Plus, we explore other important additions and changes to the standards, including a new standard on the prevention and management of chronic kidney disease and vaccination updates.
We look at the relationship between cannabis, hyperemesis, and ketoacidosis for those living with type 1 diabetes. Plus, we invite you to test your knowledge with our Question of the week based on the 2022 SOC.
Coach Beverly updated our Cheat Sheets to reflect the SOC updates so you can download these helpful references and study tools. Lastly, our 2022 medications and glucagon PocketCards are back from the printer and ready for mailing.
With the New Year, you might have set a goal or two for yourself. I hope you have success, but if not, that is okay too.
Coach Beverly, Bryanna, and Jackson
Click here to read our full December 2022 newsletter.
Featured Articles
- ADA Standards 2022 – Important Updates
- New 2022 Cheat Sheets for Screening and Insulin
- Type 1, Cannabis, and DKA
- Take the CDCES from Home Starting in 2022
- Question of the Week
- Rationale of the Week
Upcoming Webinars
- CDCES Prep | Jan 26th
- BC-ADM Prep | Feb 9th
- Diabetes Fundamentals | Begins Jan 11th
- ADA Standards| Feb 3rd
Featured Items
- CDCES Prep Bundle + Review Guide
Want to learn more about this topic?
Enroll in our Diabetes Fundamentals | Level 1
Airs Live Jan 11th – Jan 27th, 2022 at 11:30 am PST
This bundle is specifically designed for healthcare professionals who want to learn more about diabetes fundamentals for their clinical practice or for those who are studying for the Certified Diabetes Care and Education Specialist (CDCES) exam.
2022 Live Webinar Updates
- January 11, 2022 – Class 1 – Getting to the Nitty Gritty 1.5 CEs
- January 13, 2022 – Class 2 – Nutrition and Exercise 1.5 CEs
- January 18, 2022 – Class 3 – Insulin Therapy & Pattern Management 1.5 CEs
- January 20, 2022 – Class 4 – Meds Overview for Type 2 – 1.5 CEs
- January 25, 2022 – Class 5 – Goals of Care – 1.5 CEs
- January 27, 2022 – Class 6 – Hypoglycemia, Sick Days, Monitoring, Foot Care 1.5 CEs
Intended Audience: A great course for healthcare professionals in the field of diabetes education looking for a straightforward explanation of identification and treatment of hyperglycemic crises.
Instructor: Beverly Thomassian RN, MPH, CDCES, BC-ADM is a working educator and a nationally recognized diabetes expert.
All hours earned count toward your CDCES Accreditation Information
Sign up for Diabetes Blog Bytes – we post one daily Blog Byte from Monday to Friday. And of course, Tuesday is our Question of the Week. It’s Informative and FREE! Sign up below!
[yikes-mailchimp form=”1″]The use of DES products does not guarantee the successful passage of the CDCES exam. CBDCE does not endorse any preparatory or review materials for the CDCES exam, except for those published by CBDCE.
Cannabis, DKA and Vomiting? New Diagnosis Proposed

As a diabetes specialist in a rural clinic, many of my clients’ use marijuana to help them cope with chronic neuropathy.
Due to hyperemesis and other factors, people with type 1 diabetes who use cannabis on a regular basis, may present to the emergency room with diabetes ketoacidosis (DKA).
However, their unusual labs might cause some initial confusion in determining the correct diagnosis.
In a study that appeared in Diabetes Care, researchers followed people with type 1 admitted to the emergency department for DKA over a five-year period. On admission, they checked to see if they were cannabis positive. Of the 68 people with type 1 in DKA (out of 172 DKA events) who had cannabis in their system, the lab results were surprising. Usually, people in diabetes ketoacidosis have a low pH (less than 7.3) and a low bicarbonate, due to the presence of excess ketone bodies. However, for those with positive cannabis, their pH (mean 7.42 vs 7.09) and bicarbonate (mean 19.2 mmol/L vs 9.1 mmol/L) respectively, were both elevated compared to non users. But their glucose levels, anion gap and beta-hydroxybutyrate were similarly elevated in both groups.
The authors speculate that this paradoxical presentation may be due to vomiting syndromes associated with cannabis use.
Frequent marijuana use can lead to cannabinoid hyperemesis syndrome (CHS). CHS is defined as recurrent nausea, vomiting and cramping abdominal pain that is sometimes associated with at least weekly cannabis use. A common treatment for this syndrome is hot bath or shower.
With heavier marijuana use, people are at risk for cyclic vomiting syndrome (CVS), in which they experience unrelenting nausea and vomiting. The most effective treatment for this is to abstain from cannabis for at least a few weeks. People with type 1 diabetes and gastroparesis are especially at risk for both CHS and CVS. A person with type 1 and gastroparesis is also more at risk for other neuropathies and the associated chronic, often debilitating pain.
The authors are eager to share their findings and suggest screening for cannabis for those admitted with type 1 in hyperglycemic crisis, especially if the person presents with an elevated pH and bicarbonate. The researchers suggest a new term, “Hyperglycemic ketosis due to cannabis hyperemesis syndrome” or HK-CHS.
The diagnostic criteria for hyperglycemic ketosis due to cannabis hyperemesis syndrome (HK-CHS) would include:
- Elevated glucose
- Elevated anion gap
- pH of 7.4 or greater
- Bicarbonate of 15 mmol/L or greater
in the presence of ketosis in those presenting with DKA.
Due to fears of opioid addiction and with the legalization of marijuana in many states, people with diabetes are turning to cannabis to manage their chronic neuropathic pain.
As diabetes specialists, we can encourage having open and honest conversations about marijuana use. If people are experiencing excess vomiting associated with cannabis use, we can help explore other options to manage chronic pain including referral to a pain management clinic and mental health support as needed.
Want to learn more about this topic?
Level 2 | Hyperglycemic Crises, DKA & HHS Standards | 1.0 CE
Annual Webinar Recorded on December 15th
This course discusses common causes of hyperglycemia crises. Topics include hyperglycemia secondary to medications and insulin deprivation. The difference and similarities between Diabetes Ketoacidosis and Hyperosmolar Hyperglycemic Syndrome are also covered. Treatment strategies for all situations are included.
Objectives:
- Common causes of hyperglycemic crises.
- The difference and similarities between DKA and HHS and treatment strategies
- Causes and treatment of hyperglycemic crises.
Intended Audience: A great course for healthcare professionals in the field of diabetes education looking for a straightforward explanation of identification and treatment of hyperglycemic crises.
Instructor: Beverly Thomassian RN, MPH, CDCES, BC-ADM is a working educator and a nationally recognized diabetes expert.
Enroll in our entire Level 2 – Standards of Care to join us for the below Annual Live Webinar Updates. All courses air at 11:30 a.m. (PST)
- December 15, 2021 – Hyperglycemic Crises, DKA & HHS Standards | 1.0 CE
- December 21, 2021 – Assessing and Promoting Well-Being: From Population Health to a Person-Centered Approach Standards | 1.5 CEs
- February 3, 2022 – ADA Standards of Care | 2.0 CEs
- March 24, 2022 – Meds Management for Type 2 – 1.5 CEs
- March 29, 2022 – Lower Extremity Assessment 1.5 CEs
- April 26, 2022 – Microvascular Complications, Eye, Kidney Nerve Disease 1.5 CEs
- April 28, 2022 – Critical Assessment of Diabetes Patient 2.0 CEs
- May 10, 2022 – Cardiovascular Disease and Diabetes Standards 1.5 CEs
- May 12, 2022 – Older Adults and DIabetes 1.5 CEs
- May 17, 2022 – Tots to Teens – Diabetes Standards 1.5 CEs
- May 19, 2022 – Pregnancy and Diabetes 1.5 CEs
- May 26, 2022 – Hospital and Hyperglycemia 1.5 CEs
- July 21, 2022 – Setting up a Successful Diabetes Program 1.5 CEs
All hours earned count toward your CDCES Accreditation Information
Sign up for Diabetes Blog Bytes – we post one daily Blog Byte from Monday to Friday. And of course, Tuesday is our Question of the Week. It’s Informative and FREE! Sign up below!
[yikes-mailchimp form=”1″]The use of DES products does not guarantee the successful passage of the CDCES exam. CBDCE does not endorse any preparatory or review materials for the CDCES exam, except for those published by CBDCE.
Diabetes Burnout or Distress? 12 Reframes that can HELP
Let’s be honest. There is a lot of work associated with diabetes self-management. And despite best efforts, sometimes blood sugars just land in the above target or below target zone. That’s why we are trying to move away from using the term “control”, because it suggests that a person can take certain actions to get blood sugars on target all the time, and that’s just not true. At any given time, there are dozens of factors affecting blood sugar including; body temperature, stress levels, glucagon release, activity level, undigested food, metabolic rate, time since eating and many more.
Plus, diabetes self-management can be very burdensome, especially when you add on the emotional responses and expectations. Here is how a diabetes specialist, Heather Beiden Jacobs, described the burden of daily self-management.
Let’s imagine that each self-care activity is a different size rock that a person carries around in their diabetes backpack. They check their blood sugar before breakfast and it’s above target. The first rock in the backpack is pretty heavy because it holds the action of evaluating their blood sugar PLUS the emotions around the number being above their target. They take some insulin (next rock) and skip breakfast and head to work. They get low blood sugar while at a meeting and need to leave to get a snack from the vending machine (soda). This is another heavy rock, because not only did they have to manage a low, but there can also be a lot of big feelings around letting blood sugars go too low. Throughout the rest of the day, they add several more rocks to their backpack which can make things can start getting really heavy and burdensome.
If this kind of day only happens occasionally then their backpack is usually pretty light and manageable. But, if day after day the blood sugars are fluctuating a lot and the person can’t seem to get them on target, the backpack becomes very heavy and unwieldy.
That’s when the negative and judgmental emotions can creep in, these are the ones that are usually associated with feeling like they are not doing enough to manage their diabetes. That no matter what, blood sugars are “out of control”.
This can dramatically impact the daily quality of life and their ability to self-manage. A person might feel like, why bother? They might even take a diabetes vacation. We want to support people on their diabetes self-management journey and help them minimize distress and burnout. Coach Beverly listened to a bunch of great podcasts by the experts in the field and compiled a summary of the suggestions plus added in a few of her own garnered from decades of supporting people through “diabetes vacations”.
12 Reframes to Help with Diabetes Burnout or Distress
- It’s not your fault you have diabetes. It’s not your fault your pancreas doesn’t work right.
- You can’t control your blood sugars all the time, but you can take actions to manage your diabetes to the best of your ability.
- Blood sugars are not good or bad, they are just numbers that inform us of what action is needed next.
- Listen to your self-talk. It is tempting to be overly self-critical and blame ourselves. Try to imagine you are coaching a friend with diabetes. What advice or coaching would you provide?
- Diabetes isn’t about perfect or getting it right all the time. Its about taking baby steps to make small improvements and keep safe.
- Take short mental breaks from your diabetes – walk outside, enjoy a hobby, listen to music, volunteer, join a group.
- Talk about your feelings to friends and family. Let them know how to help you succeed and things that don’t help.
- Keep active, nourish your body, try meditation, enjoy oxygen cocktails, get out in nature.
- Remind yourself of all the work you ARE doing to manage your diabetes
- Join diabetes camps, social media groups, find your people, your community.
- Consider connecting with a mental health professional.
- Remember, you are not alone. You are resilient. You are not your blood sugars. You got this. Baby Steps.
Want to learn more about this topic?
Enroll in our Level 2 | Assessing and Promoting Well-Being: From Population Health to a Person-Centered Approach Standards | 1.5 CEs
Annual Update Recorded on December 21st

This presentation will include the latest information on Social Determinants of health, assessment strategies, and approaches. We will explore the psychosocial issues that can discourage individuals from adopting healthier behaviors and provides strategies to identify and overcome these barriers. Life studies are used to apply theory to real-life situations. A great course for anyone in the field of diabetes education or for those looking for a new perspective on assessment and coping strategies.
Objectives:
- State strategies to assess and address social determinants of health
- Discuss health care delivery systems using a person-centered approach
- List screening tools that can help detect depression, trauma, and cognitive decline
- Describe psycho-social and emotional barriers to diabetes self-management
- Provide strategies for healthcare professionals to identify and overcome barriers to self-care
Intended Audience: A great course for healthcare professionals in the field of diabetes education looking for a straightforward explanation of identification and treatment of hyperglycemic crises.
Instructor: Beverly Thomassian RN, MPH, CDCES, BC-ADM is a working educator and a nationally recognized diabetes expert.
Enroll in our entire Level 2 – Standards of Care to join us for the below 2022 Live Webinar Updates. All courses air at 11:30 a.m. (PST)
- December 15, 2021 – Hyperglycemic Crises, DKA & HHS Standards | 1.0 CE
- December 21, 2021 – Assessing and Promoting Well-Being: From Population Health to a Person-Centered Approach Standards | 1.5 CEs
- February 3, 2022 – ADA Standards of Care | 2.0 CEs
- March 24, 2022 – Meds Management for Type 2 – 1.5 CEs
- March 29, 2022 – Lower Extremity Assessment 1.5 CEs
- April 26, 2022 – Microvascular Complications, Eye, Kidney Nerve Disease 1.5 CEs
- April 28, 2022 – Critical Assessment of Diabetes Patient 2.0 CEs
- May 10, 2022 – Cardiovascular Disease and Diabetes Standards 1.5 CEs
- May 12, 2022 – Older Adults and DIabetes 1.5 CEs
- May 17, 2022 – Tots to Teens – Diabetes Standards 1.5 CEs
- May 19, 2022 – Pregnancy and Diabetes 1.5 CEs
- May 26, 2022 – Hospital and Hyperglycemia 1.5 CEs
- July 21, 2022 – Setting up a Successful Diabetes Program 1.5 CEs
All hours earned count toward your CDCES Accreditation Information
Sign up for Diabetes Blog Bytes – we post one daily Blog Byte from Monday to Friday. And of course, Tuesday is our Question of the Week. It’s Informative and FREE! Sign up below!
[yikes-mailchimp form=”1″]The use of DES products does not guarantee the successful passage of the CDCES exam. CBDCE does not endorse any preparatory or review materials for the CDCES exam, except for those published by CBDCE.
December eNews | Diabetes Distress & Holidays? New Handout with 12 Reframes to Help

December eNews | Diabetes Distress & Holidays? New Handout with 12 Reframes to Help
Happy December
Greetings to my wonderful health care colleagues. Thank you for all the love and care you have provided this year. I know you touch the lives and hearts of many people who boldly try their best to self-manage their diabetes and I am grateful for you!
As I am sure you have witnessed over time, holidays can amplify stress levels for people living with diabetes. With that in mind, we think this is a perfect time to provide you with some tools to address diabetes distress and burnout during the holidays and in preparation for those New Year resolutions.
Approximately 30% of people with diabetes experience distress at any given time. In addition, many people may be struggling with diabetes burnout.
As health care providers, how do we know if someone is in diabetes distress or is burning out on their self-care?
We might connect with these individuals in a hyperglycemic or hypoglycemic crisis. Maybe they are not showing up for their appointments. These individuals might be mistakenly labeled as “non-adherent” or it may be wrongly assumed that they just don’t care. However, we are compelled to reach out to them and provide a compassionate check-in of their emotional health and state of well-being.
Diabetes specialists help identify and address diabetes distress to improve quality of life and outcomes.
Read more to learn the definition and signs of diabetes distress and burnout and what action to take. Download our FREE Handouts on Surviving the Holidays and Ideas to Deal with Diabetes Distress.
We hope you can join us for our Annual Webinar Updates starting in December. We have over 50 courses to update, so Coach Bev likes to get an early start (see schedule below).
Wishing you health and moments of awe as we move toward 2022.
Coach Beverly, Bryanna, and Jackson
Click here to read our full December 2021 newsletter.
Featured Topics
- How to Identify Diabetes Distress
- 12 Ways to Help Diabetes Distress
- Coach Bev Receives Statewide World
- Question of the Week
- Rationale of the Week
Upcoming Webinars
- CDCES vs. BC-ADM | Dec 9th
- Hyperglycemic Crisis | Dec 15th
- Test Taking Toolkit | Dec 16th
- Assessing & Promoting Well-Being | Dec 9th
- Diabetes Fundamentals | Begins Jan 11th
- ADA Standards of Care | Feb 3rd
- Bootcamp | Begins Feb 8th
Featured Items
- CDCES Prep Bundle + Review Guide
- Free Resources
Test Taking Practice Exam Toolkit Webinar
20 Sample Practice Questions
Join us live June 30, 2022, for live webinar 2022 updates
You are invited to join Coach Beverly for this FREE Webinar. And, if you want to have access to an additional 220+ sample practice online questions, you can purchase the complete Test Taking Toolkit.
For many of us, taking the certification exam is a nerve-wracking process.
During this webinar, Coach Beverly will help you transform your nervousness into focused energy that will help you succeed. She will provide test-taking tips based on her experience taking the certification exam six times.
2 Ways to Join Test Taking Webinar
Watch Webinar for FREE
This includes a review of 20 sample test questions with test-taking strategies. This does not include access to the recorded webinar or the practice questions.
This includes access to the recorded version of this webinar on your Online University Student Portal. Plus, the Test Taking Toolkit provides you with over 220 sample online practice questions, simulating the exam experience. A perfect way to assess your knowledge and create a focused study plan, while increasing your test-taking confidence.
Don’t worry if you can’t make it live.
Your registration guarantees access to the recorded version.
Sign up for Diabetes Blog Bytes – we post one daily Blog Byte from Monday to Friday. And of course, Tuesday is our Question of the Week. It’s Informative and FREE! Sign up below!
[yikes-mailchimp form=”1″]Accreditation: Diabetes Education Services is an approved provider by the California Board of Registered Nursing, Provider 12640, and Commission on Dietetic Registration (CDR), Provider DI002. Since these programs are approved by the CDR it satisfies the CE requirements for the CDCES regardless of your profession.*
The use of DES products does not guarantee the successful passage of the CDCES exam. CBDCE does not endorse any preparatory or review materials for the CDCES exam, except for those published by CBDCE.